The white coat, arguably second only to a priest’s clerical collar in symbolic workplace attire, has long been associated with doctors. Originating in the late 19th century, surgeons and physicians adopted the white lab coat to distinguish themselves from less credible practitioners. But in today’s medical landscape, the White Doctor Coat evokes a range of interpretations, from professionalism and trustworthiness to elitism and a potential source of infection.
While a significant majority of medical schools (97%) hold white coat ceremonies, the actual use of white doctor coats in clinical practice varies widely across institutions and specialties. Pediatricians and psychiatrists, for instance, have voiced concerns about their use, suggesting they can be intimidating to patients. The Mayo Clinic even advises its physicians to wear only business attire, aiming to foster a more approachable doctor-patient relationship.
However, a comprehensive study conducted at the University of Michigan, involving 4,000 patients across 10 U.S. academic medical centers, revealed that physician attire significantly impacts patient perception and satisfaction. Published in BMJ Open, the research indicated that patients perceived doctors wearing a white coat over business attire (navy blue suit and dress shoes) as more knowledgeable, trustworthy, caring, and approachable. This was especially true for patients aged 65 and older. Scrubs worn under a white coat ranked second, followed by business attire alone. Interestingly, in emergency and operating room settings, scrubs alone were preferred.
Dr. Christopher Petrilli, lead author of the study and assistant professor of hospital medicine at the University of Michigan Medical School, emphasizes the ease of modifying physician attire. “At a time when we’re all trying to be more patient-centered, doesn’t it make sense to do what people want?” he questions.
The Dual Nature: Image and Infection Risk
Despite patient preferences, not everyone champions the white doctor coat. Dr. Mike Edmond, chief quality officer and clinical professor of infectious diseases at University of Iowa Hospitals and Clinics, challenges the notion that patient preference should dictate doctor’s clothing. He recounts an anecdote where a patient, needing his assistance when he was casually dressed, dismissed his apology for not wearing “doctor clothes,” stating, “I don’t care if you are in your pajamas. I just want you to help me.”
Dr. Edmond also points to substantial evidence highlighting the white coat as a potential vector for microbes, particularly around the cuffs and pockets. Following a UK study in 1991, numerous studies have corroborated the germ-harboring nature of white coats. This led the BBC to declare the white coat “more or less dead” by 2007. In 2008, the UK’s National Health Service, already wary of the white coat’s potential to create distance between doctors and patients, mandated bare-elbows for physicians who chose to wear them. The American Medical Association even considered a ban on white coats in hospitals in 2009.
 Doctor Attire Comparison: White Coat vs. Business Casual for Professional Medical Appearance
Doctor Attire Comparison: White Coat vs. Business Casual for Professional Medical Appearance
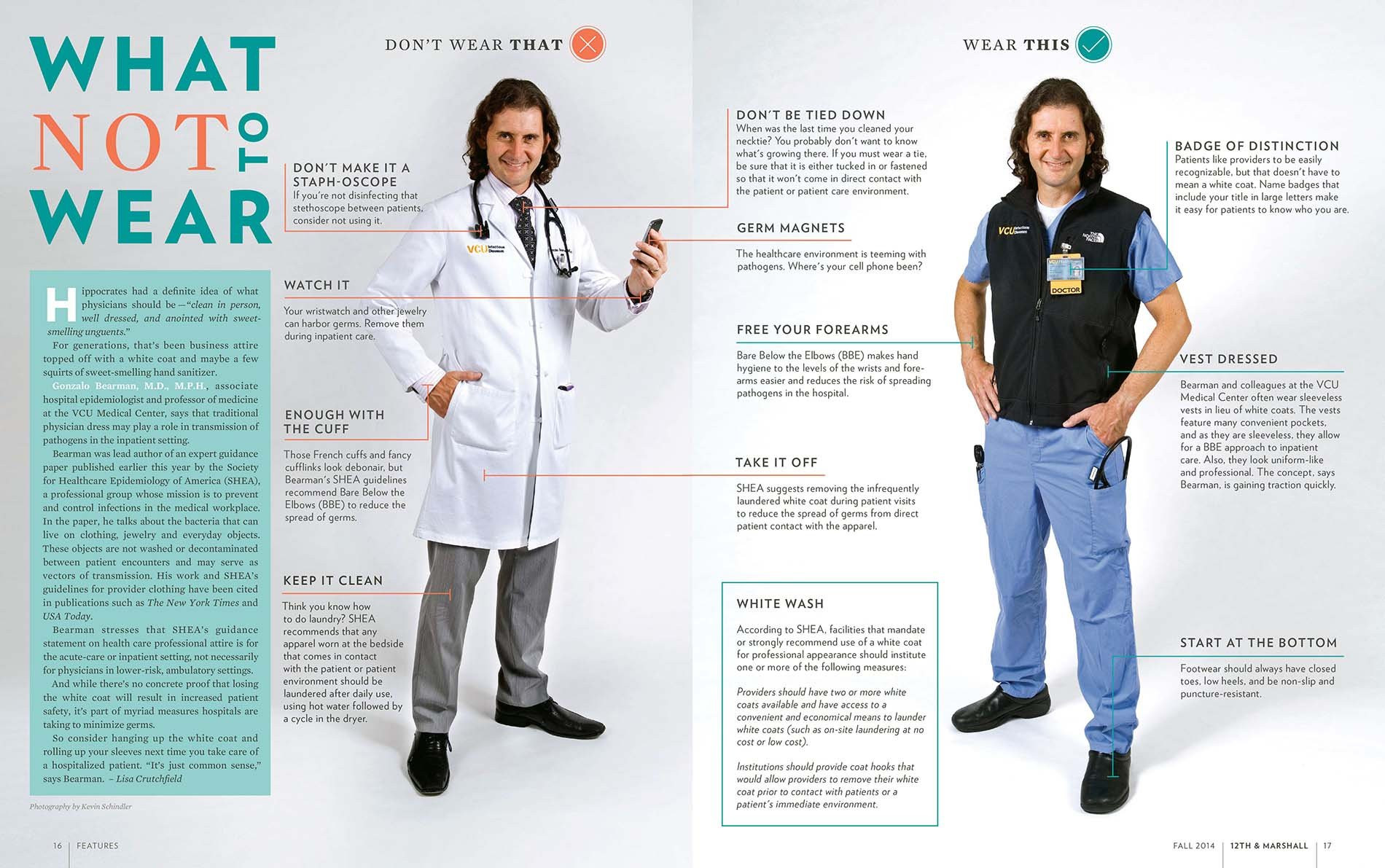
Virginia Commonwealth University School of Medicine provides guidance on doctor attire, suggesting alternatives like a sleeveless black neoprene vest to maintain professionalism without the risk of germ transmission associated with traditional white doctor coats.
One proposed solution to mitigate infection risks is more frequent laundering of white coats. However, studies reveal that doctors typically wash their lab coats infrequently, approximately every 12 days, and a significant percentage admit to rarely laundering their neckties.
Infectious disease specialists, while acknowledging the lack of direct evidence linking white coat germs to patient illness, suggest a simple solution: short sleeves. A 2017 study led by Dr. Amrita John, an infectious disease specialist at University Hospitals Cleveland Medical Center, demonstrated that long sleeves contribute to cross-contamination. The study revealed that 25% of healthcare workers wearing long-sleeved coats acquired contamination, and 5% transferred pathogens to clean surfaces.
Dr. John advocates for a balanced approach to white coats. Reflecting on her medical training in India, she notes the emphasis on minimizing barriers between doctors and patients. However, she recognizes the patient expectation for doctors to wear them. Her compromise is the short-sleeved white coat, citing both climate considerations from her training and the practical benefit of reduced pathogen transmission.
“In my medical school training in India, we didn’t want to have a barrier between patients and us. But it’s true many people expect doctors to wear [white coats].”
Dr. Amrita John, University Hospitals Cleveland Medical Center
Virginia Commonwealth University School of Medicine has proactively addressed these concerns by offering doctors a sleeveless black neoprene vest. Dr. Gonzalo Bearman, chair of the division of infectious diseases, explains that this vest fulfills the practical needs of a white coat – warmth and pockets – without the infection risks. The choice of black aligns with university colors and has resulted in a high rate of bare-below-the-elbows compliance without strict mandates. While Dr. Bearman acknowledges the lack of definitive proof of infection reduction, he considers it a sensible precaution.
Beyond Germs: White Coat Syndrome and Hierarchy
Alternatives to the traditional white coat may also address “white coat syndrome,” a phenomenon recognized since 1896. This syndrome describes the anxiety-induced elevated blood pressure readings experienced by up to 30% of patients in medical settings. Recent research underscores the seriousness of this condition, revealing a doubled mortality risk for patients with white coat hypertension compared to those with normal blood pressure.
Furthermore, the traditional hierarchy reflected in white coat length is being challenged. Historically, first-year residents wore shorter, hip-length white coats, transitioning to longer, knee-length coats after their first year. While subtle to patients, this distinction was significant within the medical community.
The Osler Medical Residency Training Program at Johns Hopkins Hospital, the oldest in the country, has abandoned this tradition. New residents voiced concerns that the short white coat symbolized a hierarchical structure, placing them below senior colleagues.
Dr. Sanjay Desai, director of the residency program at Johns Hopkins (and a white coat proponent), explains that the short coat tradition stemmed from the idea that an MD alone didn’t equate to immediate clinical expertise. The first year was considered a crucial learning period.
Students interpreted the short white coat “as a physical symbol of hierarchy and rigidity, so we eliminated it. Our values haven’t changed. But I am perfectly willing to compromise on symbols.”
Dr. Sanjay Desai, Johns Hopkins Hospital
This shift towards egalitarianism resonates with younger generations favoring casual attire and those who believe hierarchical symbols can impede patient safety. Dr. Edmond argues that coat length distinctions might discourage junior doctors from speaking up about potential errors made by senior physicians.
Will the white doctor coat disappear entirely? Unlikely. However, its role and symbolism continue to be debated within the medical profession. Dr. Paul Sax, an infectious disease specialist at Brigham and Women’s Hospital in Boston, notes the passionate responses, both for and against, he receives when discussing the topic.
Ultimately, personal preference plays a significant role. Dr. Desai, for example, values his white coat. “I don’t wear it every day,” he says, “but I do when I am in front of patients. It’s part of the process for me. It’s almost a uniform for when we want to help patients feel better.”
This enduring debate highlights the complex and evolving symbolism of the white doctor coat in modern medicine, balancing tradition and patient perception with contemporary concerns about hygiene and professional dynamics.

