Are you noticing bothersome bumps under your skin and wondering What Doctor Removes Cysts effectively? Thebootdoctor.net is here to guide you through understanding cysts and finding the right medical professional for their removal. Seeking expert help ensures proper diagnosis and treatment, leading to healthier skin. Explore the comprehensive resources at thebootdoctor.net to manage your skin health effectively, focusing on expert dermatology and specialized cyst removal.
1. What Exactly is a Cyst?
A cyst is a sac-like pocket filled with fluid, pus, or other material. It can develop in various parts of the body, including the skin, organs, and tissues. When it comes to skin cysts, these are essentially pockets filled with skin cells, bacteria, and pus. Cysts vary significantly in size, ranging from tiny, almost imperceptible bumps to larger, more noticeable masses. They can appear anywhere on the body, making it essential to understand their nature and seek appropriate medical attention.
1.1. Types of Cysts
Several types of cysts can occur on the skin, each with its unique characteristics. Here are a few common ones:
-
Epidermoid Cysts (Sebaceous Cysts): These are the most common type of skin cysts, often arising from hair follicles. They are filled with keratin, a protein found in skin cells.
-
Pilar Cysts: Similar to epidermoid cysts, pilar cysts usually develop on the scalp and are also filled with keratin.
-
Ganglion Cysts: These cysts typically form near joints or tendons, particularly in the wrist or hand. They are filled with a thick, jelly-like fluid.
-
Digital Mucous Cysts: These small, fluid-filled cysts develop on the fingers or toes, usually near the nail.
Understanding the different types of cysts is essential for proper diagnosis and treatment. Consulting a dermatologist or healthcare professional at thebootdoctor.net can help determine the specific type of cyst and the most appropriate course of action.
2. What Are the Noticeable Symptoms of a Cyst?
Cysts often manifest as small knots or kernels beneath the skin’s surface. They may originate from an infected hair follicle or acne pore, leading the skin to turn inward on itself. You may feel a bump or knot in the skin. If the cyst grows large enough, it might drain, emitting a foul odor due to the expelled skin cells.
- Visible Bump: A noticeable lump under the skin that can vary in size.
- Pain or Discomfort: Some cysts may be tender to the touch or cause pain, especially if they become inflamed or infected.
- Redness and Swelling: The skin around the cyst may appear red and swollen, indicating inflammation or infection.
- Drainage: In some cases, a cyst may rupture and drain fluid or pus, often accompanied by an unpleasant odor.
If you experience any of these symptoms, it’s essential to seek medical advice from a qualified healthcare professional at thebootdoctor.net for proper evaluation and management.
3. What Factors Contribute to the Formation of Skin Cysts?
Skin cysts typically arise when the skin turns inward on itself. Imagine the skin as a flat balloon. If there’s material inside, like skin cells, it naturally pushes outward. However, if the opening becomes blocked, these cells get trapped inside, forming a pocket. This pocket becomes a haven for cells that can’t escape, leading to cyst formation.
3.1. Common Causes of Skin Cysts
Understanding the underlying causes of skin cysts can help in prevention and appropriate management. Here are some common factors that contribute to their development:
-
Blocked Hair Follicles: One of the most common causes is the blockage of hair follicles. When dead skin cells and oil get trapped within a follicle, it can lead to the formation of a cyst.
-
Skin Trauma: Injuries to the skin, such as cuts, scrapes, or surgical incisions, can sometimes result in cyst formation. The trauma can cause skin cells to become trapped and multiply, leading to a cyst.
-
Oil Gland Dysfunction: Sebaceous glands produce oil to lubricate the skin. If these glands become damaged or blocked, it can lead to the formation of sebaceous cysts.
-
Genetic Predisposition: Some individuals may be genetically predisposed to developing cysts. If there is a family history of cysts, the likelihood of developing them may be higher.
-
Infections: Bacterial or fungal infections can sometimes trigger the formation of cysts. These infections can cause inflammation and the accumulation of fluid and debris, leading to cyst development.
4. Which Medical Professionals Specialize in Treating Cysts?
While primary care doctors and surgeons can address skin cysts, dermatologists are the specialists most commonly involved in treating and removing sebaceous and pilar cysts. Dermatologists concentrate on skin health, making cyst removal a routine part of their training and practice.
4.1. The Role of a Dermatologist
Dermatologists possess specialized knowledge and skills in diagnosing and treating various skin conditions, including cysts. Here’s how they can help:
- Diagnosis: Dermatologists can accurately diagnose the type of cyst you have through physical examination and, if necessary, a biopsy.
- Treatment Options: They offer a range of treatment options tailored to the specific type and size of the cyst.
- Surgical Removal: Dermatologists are skilled in performing surgical procedures to remove cysts safely and effectively.
- Prevention Advice: They can provide guidance on preventing future cyst formation and maintaining healthy skin.
4.2. Other Medical Professionals
While dermatologists are the primary specialists for cyst removal, other healthcare providers may also be involved in the process:
- Primary Care Physicians: Can initially assess the cyst and refer you to a dermatologist if necessary.
- Surgeons: May be consulted for larger or more complicated cysts that require extensive surgical removal.
Choosing the right medical professional is crucial for effective cyst management. Dermatologists, with their specialized expertise, are often the best choice for diagnosing and treating skin cysts. thebootdoctor.net can provide resources to help you find qualified dermatologists and healthcare professionals in your area.
 cyst removal procedure
cyst removal procedure
5. What Are the Standard Methods Used by Dermatologists to Remove a Cyst?
Dermatologists employ outpatient procedures to remove cysts, opting for lancing if the cyst has ruptured. If the cyst is intact, they typically excise it.
5.1. Lancing a Cyst
Lancing involves making a small incision in the cyst with a sharp blade, followed by draining its contents. While this method is sometimes seen in online cyst-popping videos, it’s not always the best for permanent removal. However, if a cyst has already ruptured, lancing can help remove most of its contents.
- Procedure: A sharp blade is used to create an opening in the cyst.
- Drainage: The contents of the cyst are squeezed out.
- Considerations: This method is best for cysts that have already ruptured.
- Limitations: Lancing alone may not prevent the cyst from reforming.
In these cases, it’s crucial to remove the sac around the contents to prevent recurrence. If the lining of the cyst wall isn’t removed, the cyst will likely return.
5.2. Excising a Cyst
Excising is typically the preferred removal method when the cyst is intact. This involves making an elliptical incision around the cyst to remove the entire cyst wall and its contents. The area is then stitched up to heal.
- Procedure: An elliptical incision is made around the cyst.
- Removal: The entire cyst wall and contents are removed.
- Closure: The area is stitched up to promote healing.
- Benefits: Excising reduces the likelihood of the cyst recurring.
6. Why Is Professional Dermatological Cyst Removal Recommended Over DIY Methods?
Attempting at-home cyst removals is generally not recommended, despite the availability of numerous DIY videos online. Squeezing or lancing cysts yourself can lead to complications and is unlikely to provide a permanent solution.
6.1. Risks of At-Home Cyst Removal
Trying to remove cysts at home can worsen the problem and lead to several complications:
- Infection: Breaking the skin without proper sterilization can introduce bacteria and lead to infection.
- Scarring: Improper techniques can damage the skin and increase the risk of scarring.
- Recurrence: Squeezing the cyst without removing the sac will likely result in the cyst refilling and recurring.
- Inflammation: Aggressive squeezing can cause inflammation and make the condition worse.
6.2. Benefits of Professional Removal
Professional cyst removal by a dermatologist offers several advantages:
- Complete Removal: Dermatologists ensure the entire cyst sac is removed, reducing the chance of recurrence.
- Sterile Environment: Procedures are performed in a sterile environment to minimize the risk of infection.
- Proper Technique: Dermatologists use precise techniques to minimize scarring and ensure optimal healing.
- Expert Assessment: They can accurately diagnose the cyst and recommend the most appropriate treatment.
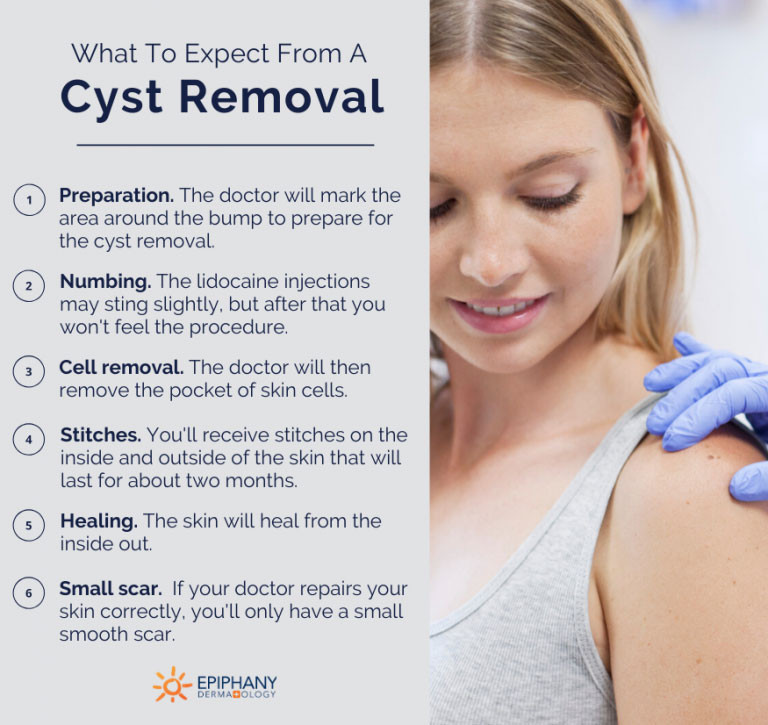
7. What Can You Expect During a Professional Cyst Removal Procedure?
During a cyst removal procedure, the doctor will begin by marking and numbing the area around the bump. You’ll receive Lidocaine injections, which may cause a slight sting, but this is usually the most uncomfortable part. After that, you shouldn’t feel any pain during the procedure. The dermatologist will then remove the pocket of skin cells and place stitches on the inside and outside of the skin, which will remain for about two months as the skin heals from the inside out.
7.1. Step-by-Step Overview
Here’s a detailed breakdown of what to expect during a professional cyst removal:
- Preparation: The area around the cyst is cleaned and prepped for the procedure.
- Anesthesia: A local anesthetic, such as Lidocaine, is injected to numb the area.
- Incision: The dermatologist makes a small incision around the cyst.
- Removal: The cyst and its contents are carefully removed, ensuring the entire sac is extracted.
- Closure: The incision is closed with stitches, which may be placed both inside and outside the skin.
- Dressing: A sterile dressing is applied to protect the area and promote healing.
7.2. Post-Procedure Care
After the cyst is removed, proper aftercare is essential to ensure optimal healing:
- Keep the Area Clean: Gently clean the area with soap and water as directed by your dermatologist.
- Apply Antibiotic Ointment: Use an antibiotic ointment to prevent infection.
- Change Dressings: Change the dressing regularly as instructed.
- Avoid Strenuous Activity: Refrain from activities that could strain the area.
- Follow-Up: Attend any scheduled follow-up appointments to monitor healing.
8. What is the Typical Healing Timeline Following Cyst Removal?
The healing process after cyst removal depends on the type of procedure performed. If the cyst was lanced, the wound will be left open to heal from the inside out. It may continue to drain after the procedure, and you should watch for any signs of the cyst reforming. If the cyst was excised, you’ll have stitches to minimize scarring. Patients may experience tenderness and mild pain, which can be managed with over-the-counter pain medication.
8.1. Factors Influencing Healing Time
Several factors can affect the healing time after cyst removal:
- Type of Procedure: Excision typically results in a quicker healing time compared to lancing.
- Size and Location of the Cyst: Larger cysts and those in areas with more movement may take longer to heal.
- Overall Health: Individuals with underlying health conditions may experience slower healing.
- Adherence to Aftercare Instructions: Following your dermatologist’s instructions is crucial for optimal healing.
8.2. Potential Complications
While cyst removal is generally safe, potential complications can occur:
- Infection: Signs include increased pain, redness, swelling, and pus.
- Scarring: Some scarring is normal, but excessive scarring can be minimized with proper technique and aftercare.
- Recurrence: If the entire cyst sac is not removed, the cyst may recur.
- Nerve Damage: Rarely, nerve damage can occur, leading to numbness or tingling in the area.
9. Does Insurance Generally Provide Coverage for Cyst Removal Procedures?
Insurance typically covers cyst removals since it’s considered a medical procedure rather than cosmetic. The costs usually go towards your deductible. However, exact costs depend on your insurance plan and whether you’ve met your deductible. Remember, you’ll need to pay out-of-pocket if you haven’t met your deductible, but cyst removal costs usually count towards that amount.
9.1. Understanding Insurance Coverage
Navigating insurance coverage for medical procedures can be complex. Here are some key points to consider:
- Medical Necessity: Insurance companies typically cover procedures deemed medically necessary.
- Deductible: You may need to meet your deductible before insurance coverage kicks in.
- Co-pay: Some insurance plans require a co-pay for each visit or procedure.
- Pre-authorization: Certain procedures may require pre-authorization from your insurance provider.
9.2. Steps to Verify Coverage
To ensure you understand your insurance coverage for cyst removal, follow these steps:
- Contact Your Insurance Provider: Call your insurance company to inquire about your coverage for cyst removal.
- Ask About Deductibles and Co-pays: Understand how your deductible and co-pay will affect your out-of-pocket costs.
- Inquire About Pre-authorization: Determine if pre-authorization is required for the procedure.
- Check with Your Dermatologist’s Office: The billing department at your dermatologist’s office can also help verify your coverage.
10. What Actions Should Be Taken if a Cyst Ruptures Unexpectedly?
If a cyst pops on its own, it can be painful and ineffective to try to squeeze and drain it yourself. It’s best to seek care from a physician, who can better remove all the contents from the cyst, ensuring it heals properly and has a lower chance of recurring. Additionally, they can provide numbing medication to minimize pain during the lancing procedure.
10.1. Immediate Steps
If a cyst ruptures on its own, take the following immediate steps:
- Wash Your Hands: Before touching the area, wash your hands thoroughly with soap and water.
- Clean the Area: Gently clean the ruptured cyst with mild soap and water.
- Apply a Sterile Dressing: Cover the area with a sterile bandage to protect it from infection.
10.2. Medical Evaluation
Seeking medical attention is crucial for proper management:
- Consult a Physician: Schedule an appointment with a doctor or dermatologist as soon as possible.
- Professional Cleaning: The doctor can thoroughly clean the area and remove any remaining debris.
- Antibiotics: If there are signs of infection, the doctor may prescribe antibiotics.
- Proper Closure: The doctor can ensure the area heals properly to minimize scarring and recurrence.
11. How Can You Determine if a Bump is Indeed a Cyst?
If you feel a hard lump under your skin, it’s important to have it checked out as soon as possible. While it might be a normal cyst that’s easily removable, it could also be something else.
11.1. Self-Examination
Regular self-examination can help you detect potential cysts early. Here’s what to look for:
- Location: Note where the lump is located on your body.
- Size: Measure the size of the lump.
- Shape: Observe the shape and contour of the lump.
- Consistency: Gently feel the lump to determine its consistency (e.g., soft, firm, hard).
- Pain: Note if the lump is painful to the touch.
11.2. Professional Diagnosis
A professional diagnosis from a healthcare provider is essential for accurate identification:
- Physical Examination: The doctor will perform a thorough physical examination of the lump.
- Medical History: They will ask about your medical history and any relevant symptoms.
- Biopsy: In some cases, a biopsy may be necessary to determine the nature of the lump.
- Imaging Tests: Imaging tests, such as ultrasound or MRI, may be used to further evaluate the lump.
12. What Recent Advances Have Been Made in Cyst Removal Techniques?
Advancements in cyst removal techniques continue to improve outcomes, reduce scarring, and enhance patient comfort. Here are some notable recent developments:
| Technique | Description | Benefits |
|---|---|---|
| Punch Biopsy Excision | Uses a small, circular blade to remove the cyst, minimizing the incision size. | Reduced scarring, quicker healing time, suitable for smaller cysts. |
| Laser Ablation | Employs laser technology to vaporize the cyst, leaving minimal damage to surrounding tissue. | Precise removal, reduced bleeding, minimal scarring, ideal for superficial cysts. |
| Minimal Incision Excision | Involves making a very small incision to remove the cyst, often using specialized instruments. | Reduced scarring, faster recovery, suitable for cysts in cosmetically sensitive areas. |
| Triamcinolone Injections | Injects triamcinolone (a corticosteroid) into the cyst to reduce inflammation and size, often used for cysts that are inflamed. | Non-surgical option, reduces inflammation, can shrink the cyst, may avoid the need for excision. |
| Ultrasound-Guided Aspiration | Uses ultrasound imaging to guide the aspiration (drainage) of the cyst, ensuring complete removal of fluid. | Precise drainage, reduces the risk of recurrence, particularly useful for ganglion cysts. |
These advances reflect ongoing efforts to improve the effectiveness and patient experience of cyst removal procedures. Consulting with a dermatologist at thebootdoctor.net can help you determine which technique is best suited for your specific condition.
FAQ About Cyst Removal
1. What is a cyst and how is it different from a tumor?
A cyst is a closed sac-like structure filled with fluid, pus, or semi-solid material, whereas a tumor is an abnormal mass of tissue that can be solid or partially filled with fluid.
2. Can a cyst disappear on its own?
Yes, some small cysts may disappear on their own, but larger or more persistent cysts usually require medical intervention.
3. Is cyst removal painful?
No, cyst removal is typically performed under local anesthesia, so you should not feel pain during the procedure.
4. How long does it take to recover from cyst removal?
Recovery time varies depending on the size and location of the cyst, but most people recover within a few weeks.
5. Are there any risks associated with cyst removal?
Yes, potential risks include infection, scarring, and nerve damage, but these are rare when the procedure is performed by a qualified dermatologist.
6. Can a cyst grow back after removal?
Yes, if the entire cyst sac is not removed, it can grow back, which is why it’s important to have the procedure done by a skilled professional.
7. How can I prevent cysts from forming?
Maintaining good hygiene, avoiding skin injuries, and managing underlying conditions can help prevent cyst formation.
8. What should I do if my cyst becomes infected?
If your cyst becomes infected, seek medical attention immediately for antibiotics and proper wound care.
9. Are there any home remedies for cysts that actually work?
While some home remedies may provide temporary relief, they are not a substitute for professional medical treatment and may lead to complications.
10. When should I see a doctor about a cyst?
You should see a doctor if the cyst is painful, growing rapidly, infected, or causing significant discomfort.
At thebootdoctor.net, we understand the importance of reliable and accessible information regarding foot and skin health. Our goal is to provide you with the knowledge and resources you need to make informed decisions about your care. Remember, proper diagnosis and treatment are essential for maintaining healthy feet and skin.

