Boils can be uncomfortable and sometimes concerning, so knowing when you should see a doctor for a boil is vital for your health and wellbeing; visit thebootdoctor.net for reliable insights into skin infections and expert foot care solutions. Early intervention can prevent complications and ensure proper treatment, promoting faster healing and minimizing discomfort, focusing on boils, skin infections and foot health.
1. What Are Boils and Why Do They Occur?
Boils are painful, pus-filled bumps that form under the skin when hair follicles become infected with bacteria. A boil starts as a small, red, tender area that can grow over a few days into a firm, painful lump. According to the American Academy of Dermatology, boils typically result from a Staphylococcus aureus (staph) infection.
1.1 Understanding Furuncles and Carbuncles
A single infected hair follicle is known as a furuncle, while a cluster of connected, infected follicles is called a carbuncle. Carbuncles are typically larger and more severe than single boils and often require medical treatment.
1.2 Common Locations for Boils
Boils can appear anywhere on the body, but they are most common in areas with hair and where there is friction, such as:
- Face and Neck
- Armpits
- Groin Area
- Inner Thighs
- Buttocks
 A photo showing a boil thats formed on a persons jawline
A photo showing a boil thats formed on a persons jawline
This image depicts a boil caused by an infected hair follicle on the jawline, highlighting the visible inflammation and localized nature of the infection.
2. What Are the Symptoms of a Boil?
Recognizing the symptoms of a boil is essential for determining the appropriate course of action.
2.1 Initial Symptoms
The initial symptoms of a boil include:
- A small, red, tender bump on the skin.
- Surrounding skin may be swollen and red.
2.2 Progressive Symptoms
As a boil develops, you may notice:
- Increased pain and tenderness.
- The lump fills with pus, forming a white or yellow center.
- The boil may drain pus.
2.3 Systemic Symptoms
In some cases, particularly with larger or multiple boils, you may experience:
- Fever
- Fatigue
- General feeling of unwellness
3. What Causes Boils?
Boils are primarily caused by bacterial infections, typically from Staphylococcus aureus bacteria.
3.1 Bacterial Infection
Staph bacteria are commonly found on the skin and in the nose of healthy individuals. Problems arise when these bacteria enter the body through a cut, scrape, or insect bite, leading to infection.
3.2 Risk Factors
Several factors can increase your risk of developing boils:
- Close Contact with Someone Who Has a Staph Infection: Sharing towels, razors, or other personal items can spread bacteria.
- Weakened Immune System: Conditions or medications that suppress the immune system make it harder to fight off infections.
- Diabetes: High blood sugar levels can impair immune function and increase the risk of skin infections.
- Poor Hygiene: Inadequate hygiene practices can allow bacteria to thrive on the skin.
- Skin Conditions: Conditions that cause breaks in the skin, such as eczema or psoriasis, can increase the risk of infection.
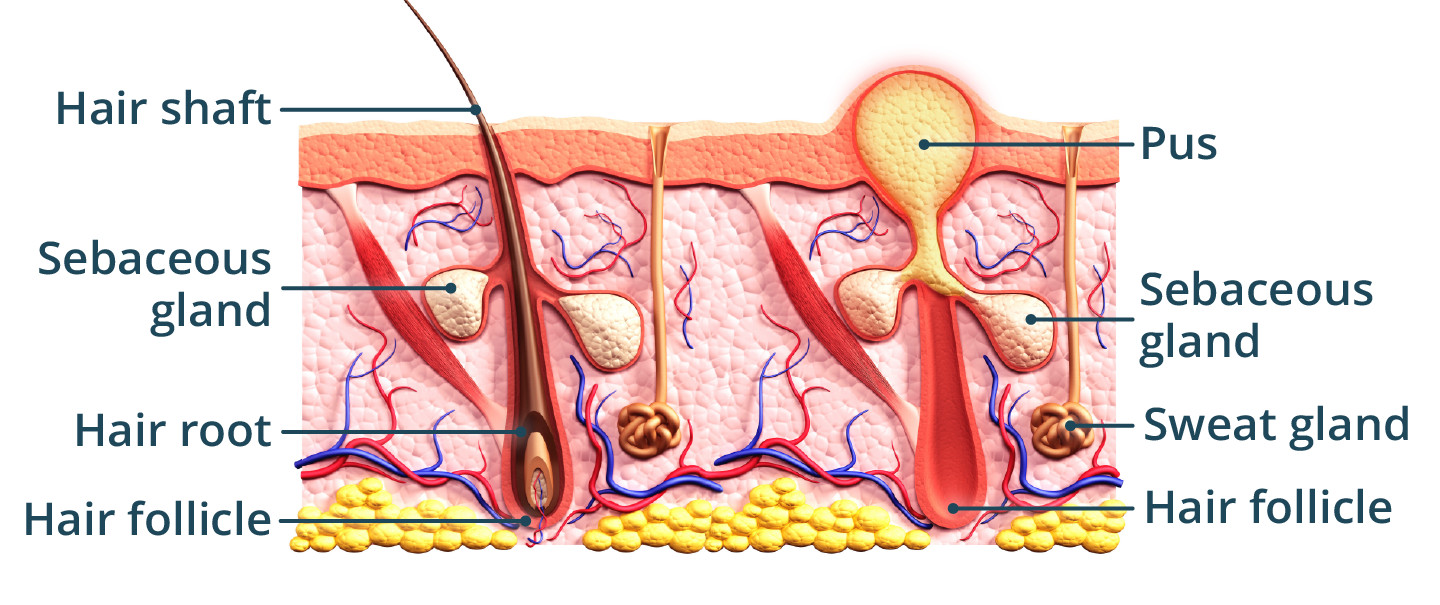 An illustration showing a healthy hair follicle on the left, compared to one infected on the right. Leading to a pus filled lump.
An illustration showing a healthy hair follicle on the left, compared to one infected on the right. Leading to a pus filled lump.
This illustration compares a healthy hair follicle with an infected one, resulting in a pus-filled lump, emphasizing the infection process.
4. When Is It Necessary to See a Doctor for a Boil?
While many small boils can be managed at home, it’s crucial to know when to seek medical attention. The American Academy of Dermatology recommends seeing a doctor if certain conditions are met.
4.1 Boils on the Face
Boils located on the face, especially around the nose or eyes, should be evaluated by a doctor. Infections in this area can potentially spread to the brain, leading to serious complications.
4.2 Large Boils
Large boils, particularly carbuncles, often require professional treatment. These may need to be lanced and drained by a healthcare provider, along with antibiotic therapy to clear the infection.
4.3 Boils Accompanied by Fever or Other Systemic Symptoms
If you experience a fever, chills, or other signs of systemic illness in addition to a boil, seek medical attention. These symptoms could indicate that the infection has spread beyond the local area.
4.4 Boils That Don’t Improve with Home Treatment
If a boil does not show signs of improvement after a week of home treatment, it’s time to see a doctor. Persistent or worsening boils may require antibiotics or other medical interventions.
4.5 Boils in Individuals with Underlying Health Conditions
People with diabetes, weakened immune systems, or other underlying health conditions should seek medical care for boils. These individuals are at higher risk of complications from infections.
4.6 Painful Boils
Boils that cause intense pain may require medical intervention to alleviate discomfort and prevent further complications. A doctor can assess the boil and determine the best course of treatment.
4.7 Boils That Recur
Recurrent boils, or boils that keep coming back, can indicate an underlying issue that needs to be addressed by a healthcare provider. Chronic boils may be a sign of MRSA or other resistant bacterial infections.
5. How Are Boils Diagnosed?
Diagnosing a boil typically involves a physical examination by a healthcare provider.
5.1 Physical Examination
During the examination, the doctor will assess the size, location, and appearance of the boil. They may also check for signs of surrounding inflammation or infection.
5.2 Swab Culture
If there is drainage from the boil, the doctor may collect a sample to send for culture. This can help identify the specific bacteria causing the infection and guide antibiotic selection.
5.3 Blood Tests
In some cases, blood tests may be ordered to evaluate the extent of the infection or to rule out other underlying conditions.
6. What Treatment Options Are Available for Boils?
Treatment for boils depends on their size, severity, and location. The goal of treatment is to eliminate the infection and promote healing.
6.1 Home Care
Small boils can often be managed with home care measures.
- Warm Compresses: Applying warm compresses to the boil for 10-15 minutes, several times a day, can help promote drainage and relieve pain.
- Hygiene: Keep the area clean by washing it gently with soap and water.
- Avoid Squeezing: Never squeeze or attempt to pop a boil, as this can spread the infection.
6.2 Medical Treatment
Larger or more severe boils may require medical intervention.
- Incision and Drainage: A doctor can lance the boil and drain the pus. This procedure provides immediate relief and helps promote healing.
- Antibiotics: Antibiotics may be prescribed to treat the infection, especially if it has spread beyond the local area.
- Wound Care: After lancing and draining, the doctor will provide instructions on how to care for the wound to prevent further infection.
7. What Are the Potential Complications of Boils?
While most boils resolve without complications, some can lead to more serious problems.
7.1 Cellulitis
Cellulitis is a bacterial infection of the skin and underlying tissues. It can occur if the infection from a boil spreads.
7.2 Sepsis
Sepsis is a life-threatening condition that occurs when the body’s response to an infection spirals out of control. Boils can lead to sepsis if the infection enters the bloodstream.
7.3 Scarring
Large boils or carbuncles can leave scars on the skin after healing.
7.4 MRSA Infection
Methicillin-resistant Staphylococcus aureus (MRSA) is a type of staph bacteria that is resistant to many antibiotics. Boils caused by MRSA can be difficult to treat.
7.5 Spread of Infection
Infections from boils can spread to other parts of the body or to other people through close contact.
8. How Can Boils Be Prevented?
Preventing boils involves practicing good hygiene and taking steps to minimize the risk of infection.
8.1 Good Hygiene
Wash your hands regularly with soap and water, especially after touching surfaces in public places.
8.2 Avoid Sharing Personal Items
Do not share towels, razors, or other personal items with others.
8.3 Proper Wound Care
Clean and cover any cuts, scrapes, or insect bites to prevent infection.
8.4 Strengthen Immune System
Maintain a healthy lifestyle, including a balanced diet, regular exercise, and adequate sleep, to strengthen your immune system.
8.5 Avoid Irritating Skin
Avoid wearing tight clothing or using harsh chemicals that can irritate the skin.
9. The Role of Diet and Lifestyle in Preventing Boils
Diet and lifestyle play a significant role in maintaining overall health and preventing skin infections like boils.
9.1 Boost Immune System
A diet rich in vitamins, minerals, and antioxidants can help strengthen the immune system and reduce the risk of infections.
9.2 Hydration
Staying hydrated helps maintain healthy skin and supports the body’s natural defenses against infection.
9.3 Manage Blood Sugar Levels
For individuals with diabetes, managing blood sugar levels is crucial for preventing skin infections.
9.4 Exercise Regularly
Regular exercise helps improve circulation and strengthens the immune system.
10. What Are the Psychological Effects of Having Boils?
Having boils can have psychological effects, including:
10.1 Self-Consciousness
Boils can be visible and unsightly, leading to feelings of self-consciousness and embarrassment.
10.2 Anxiety
Individuals with recurrent boils may experience anxiety about future outbreaks.
10.3 Social Isolation
Some people may avoid social situations due to concerns about their appearance or the risk of spreading infection.
10.4 Depression
Chronic skin conditions like boils can contribute to feelings of depression.
11. Understanding MRSA and Its Connection to Boils
MRSA (Methicillin-resistant Staphylococcus aureus) is a type of staph bacteria that is resistant to many antibiotics.
11.1 Transmission
MRSA can be transmitted through direct contact with an infected person or contaminated surfaces.
11.2 Risk Factors
Individuals who are hospitalized, have weakened immune systems, or use antibiotics are at higher risk of MRSA infection.
11.3 Treatment
MRSA infections can be difficult to treat, often requiring specialized antibiotics and wound care.
12. Boils vs. Other Skin Conditions
It’s important to differentiate boils from other skin conditions that may appear similar.
12.1 Acne
Acne is a common skin condition characterized by pimples, blackheads, and whiteheads. Unlike boils, acne is not typically caused by a bacterial infection.
12.2 Cysts
Cysts are closed sacs filled with fluid or other material. They can sometimes resemble boils but are usually not painful or inflamed.
12.3 Folliculitis
Folliculitis is an inflammation of hair follicles that can cause small, red bumps on the skin. It can sometimes be mistaken for boils.
12.4 Insect Bites
Insect bites can cause red, itchy bumps on the skin that may resemble boils. However, insect bites are usually accompanied by itching and may have a visible puncture mark.
13. Expert Advice on Managing Boils
Here is some expert advice from dermatologists and healthcare professionals on managing boils:
13.1 Do Not Squeeze
Resist the urge to squeeze or pop a boil, as this can spread the infection and lead to complications.
13.2 Keep Clean
Keep the area around the boil clean and dry to prevent further infection.
13.3 Use Warm Compresses
Apply warm compresses to the boil several times a day to promote drainage and relieve pain.
13.4 Seek Medical Attention
If the boil is large, painful, or accompanied by fever, seek medical attention promptly.
13.5 Follow Doctor’s Instructions
Follow your doctor’s instructions carefully regarding wound care and medication.
14. Real-Life Experiences
Sharing real-life experiences can provide valuable insights and support for individuals dealing with boils.
14.1 Patient Testimonials
Include quotes from patients who have successfully managed boils, sharing their experiences and tips for others.
14.2 Case Studies
Present case studies of individuals with boils, highlighting the challenges they faced and the treatments that worked for them.
15. Emerging Treatments and Research
Stay informed about the latest advancements in the treatment and prevention of boils.
15.1 New Antibiotics
Research into new antibiotics and alternative therapies for treating MRSA and other resistant bacterial infections.
15.2 Preventive Measures
Studies on preventive measures, such as antimicrobial washes and vaccines, to reduce the risk of skin infections.
16. Practical Tips for Living with Boils
Living with boils can be challenging, but here are some practical tips to help manage the condition:
16.1 Wear Loose Clothing
Wear loose-fitting clothing to avoid irritating the skin around the boil.
16.2 Avoid Friction
Avoid activities that cause friction or pressure on the affected area.
16.3 Use Antibacterial Soap
Use antibacterial soap to wash the area around the boil and prevent further infection.
16.4 Stay Positive
Maintain a positive attitude and focus on self-care to cope with the psychological effects of having boils.
17. What Is The Cost of Treating Boils?
The cost of treating boils can vary depending on the severity of the condition and the type of treatment required.
17.1 Home Care
Home care measures, such as warm compresses and over-the-counter pain relievers, are generally inexpensive.
17.2 Medical Treatment
Medical treatment, such as incision and drainage or antibiotics, can be more costly. The exact cost will depend on factors such as insurance coverage and the healthcare provider’s fees.
18. Resources and Support for People with Boils
There are many resources and support available for people with boils.
18.1 Online Forums
Online forums and support groups can provide a sense of community and allow individuals to share their experiences and tips for managing boils.
18.2 Healthcare Professionals
Healthcare professionals, such as dermatologists and primary care physicians, can provide expert advice and treatment for boils.
18.3 Educational Materials
Educational materials, such as brochures and websites, can provide valuable information about boils and how to prevent them.
19. FAQ Section
19.1 Are Boils Contagious?
Yes, boils are contagious. The bacteria that cause boils can spread through direct contact with an infected person or contaminated surfaces.
19.2 Can Boils Go Away on Their Own?
Small boils may go away on their own with home care measures. However, larger or more severe boils may require medical treatment.
19.3 How Long Do Boils Last?
Boils typically last for one to three weeks. With proper treatment, they should heal within a few weeks.
19.4 Can I Pop a Boil Myself?
No, you should not pop a boil yourself. Squeezing or popping a boil can spread the infection and lead to complications.
19.5 What Are the Signs of a Serious Boil?
Signs of a serious boil include fever, chills, red streaks around the boil, and increased pain or swelling.
19.6 Can Boils Cause Permanent Damage?
Boils can cause permanent damage, such as scarring, if they are large or severe.
19.7 What Should I Do If My Boil Keeps Coming Back?
If your boil keeps coming back, you should see a doctor to determine the underlying cause and receive appropriate treatment.
19.8 How Can I Prevent Boils in the Future?
You can prevent boils in the future by practicing good hygiene, avoiding sharing personal items, and taking steps to strengthen your immune system.
19.9 Is It Safe to Exercise with a Boil?
It is generally safe to exercise with a boil, but you should avoid activities that cause friction or pressure on the affected area.
19.10 Are There Any Natural Remedies for Boils?
Some natural remedies for boils include turmeric, tea tree oil, and garlic. However, these remedies should be used with caution and are not a substitute for medical treatment.
20. Conclusion
Knowing when you should see a doctor for a boil is crucial for ensuring timely and effective treatment. By understanding the symptoms, causes, and potential complications of boils, you can take proactive steps to manage this common skin condition and protect your health. If you are looking for reliable advice and expert solutions for foot and skin health, visit thebootdoctor.net for more information. Proper boil management, skin infection prevention, and comprehensive foot health strategies will help you maintain overall well-being.
For expert care and reliable information, contact us at:
- Address: 6565 Fannin St, Houston, TX 77030, United States
- Phone: +1 (713) 791-1414
- Website: thebootdoctor.net
Take control of your health today by visiting thebootdoctor.net, exploring our resources, and contacting us for personalized advice and treatment options!

