Are you experiencing bone, joint, or muscle discomfort and wondering who to turn to? A bone doctor, also known as an orthopedic doctor or orthopedist, specializes in the musculoskeletal system. At thebootdoctor.net, we provide clear, reliable information about bone health, helping you understand your treatment options and find the right specialist for your needs. We’ll also touch on podiatrists, rheumatologists, and osteopaths, offering a comprehensive guide to musculoskeletal healthcare.
1. What Exactly Is a Bone Doctor Called?
A bone doctor is primarily called an orthopedic doctor or orthopedist. These medical professionals specialize in the musculoskeletal system, which includes bones, joints, ligaments, tendons, muscles, and nerves.
Orthopedic doctors can diagnose and treat a wide range of conditions, from fractures and arthritis to sports injuries and congenital disorders. According to the American Academy of Orthopaedic Surgeons (AAOS), orthopedic surgeons perform approximately 6.6 million musculoskeletal procedures each year in the United States.
1.1. Delving Deeper: The Role of an Orthopedic Doctor
Orthopedic doctors are trained to address a variety of musculoskeletal issues. Their expertise covers both surgical and non-surgical treatments. They may recommend physical therapy, medication, injections, or lifestyle modifications before considering surgery.
Here’s a closer look at what an orthopedic doctor does:
- Diagnosis: They evaluate patients’ conditions using physical exams, imaging tests (X-rays, MRIs, CT scans), and other diagnostic tools.
- Treatment: They develop personalized treatment plans that may include medication, physical therapy, braces, injections, or surgery.
- Rehabilitation: They guide patients through the rehabilitation process to help them regain strength, mobility, and function.
- Prevention: They educate patients about injury prevention strategies and healthy lifestyle choices.
1.2. Subspecialties Within Orthopedics
Within the field of orthopedics, many doctors choose to specialize in a specific area. This allows them to develop advanced expertise in treating particular conditions or body parts. Some common orthopedic subspecialties include:
- Sports Medicine: Focuses on the treatment and prevention of injuries related to sports and exercise.
- Joint Replacement: Specializes in surgical procedures to replace damaged joints with artificial implants.
- Spine Surgery: Addresses conditions affecting the spine, such as herniated discs, spinal stenosis, and scoliosis.
- Hand Surgery: Treats injuries and conditions affecting the hand, wrist, and forearm.
- Foot and Ankle Surgery: Specializes in the diagnosis and treatment of foot and ankle problems.
- Pediatric Orthopedics: Focuses on the musculoskeletal health of children.
- Orthopedic Oncology: Deals with the diagnosis and treatment of bone and soft tissue tumors.
1.3. The Difference Between an Orthopedist and an Orthopedic Surgeon
While the terms “orthopedist” and “orthopedic surgeon” are often used interchangeably, there is a subtle difference. An orthopedist is a medical doctor who specializes in the musculoskeletal system. An orthopedic surgeon is an orthopedist who is also trained and qualified to perform surgical procedures.
All orthopedic surgeons are orthopedists, but not all orthopedists are orthopedic surgeons. Some orthopedists may focus on non-surgical treatments, while others may perform surgery as part of their practice.
2. When Should You See a Bone Doctor?
Knowing when to seek the expertise of a bone doctor is crucial for timely and effective treatment. It’s best to consult with an orthopedic specialist if you experience any of the following:
- Persistent pain: Pain that lasts for several weeks or months, especially if it doesn’t improve with home remedies.
- Limited range of motion: Difficulty moving a joint or limb through its full range of motion.
- Swelling, redness, or warmth: Signs of inflammation around a joint or bone.
- Deformity: A visible change in the shape of a bone or joint.
- Numbness or tingling: Sensations that may indicate nerve compression or damage.
- Instability: A feeling that a joint is giving way or unstable.
- Difficulty performing daily activities: Problems with walking, climbing stairs, lifting objects, or other everyday tasks.
- Sports-related injuries: Sprains, strains, fractures, dislocations, and other injuries sustained during athletic activities.
- Chronic conditions: Arthritis, osteoporosis, and other long-term conditions affecting the musculoskeletal system.
2.1. Specific Symptoms That Warrant a Visit
To be more specific, here are some symptoms that should prompt you to see a bone doctor:
| Symptom | Possible Underlying Condition |
|---|---|
| Sharp, shooting pain | Nerve impingement, fracture, or acute injury |
| Dull, aching pain | Arthritis, overuse injury, or chronic inflammation |
| Pain that worsens with activity | Stress fracture, tendonitis, or joint instability |
| Pain that improves with rest | Overuse injury, mild sprain, or muscle strain |
| Stiffness in the morning | Arthritis, especially rheumatoid arthritis |
| Clicking or popping in a joint | Ligament tear, cartilage damage, or joint instability |
| Locking of a joint | Meniscus tear, loose body in the joint, or joint dislocation |
| Visible bump or lump | Bone spur, ganglion cyst, or tumor |
| Inability to bear weight | Fracture, dislocation, or severe ligament tear |
2.2. The Importance of Early Diagnosis and Treatment
Seeking early diagnosis and treatment from a bone doctor can significantly improve your outcome. Delaying treatment can lead to:
- Chronic pain: Pain that persists for months or years, even after the initial injury has healed.
- Reduced function: Loss of mobility, strength, and coordination.
- Joint damage: Progression of arthritis and other degenerative conditions.
- Deformity: Changes in the shape of bones and joints that can affect appearance and function.
- Disability: Inability to perform daily activities, work, or participate in recreational activities.
According to a study published in the Journal of Bone and Joint Surgery, early intervention for certain orthopedic conditions, such as hip dysplasia in infants, can prevent the need for more extensive surgery later in life.
2.3. When to Consider Emergency Care
In some cases, a bone injury may require immediate emergency care. Seek emergency medical attention if you experience any of the following:
- Open fracture: A broken bone that protrudes through the skin.
- Severe deformity: A bone or joint that is obviously out of alignment.
- Loss of sensation or movement: Inability to feel or move a limb.
- Signs of shock: Rapid heartbeat, shallow breathing, dizziness, or loss of consciousness.
- Severe bleeding: Uncontrolled bleeding from a wound near a broken bone.
3. What Conditions Do Bone Doctors Treat?
Orthopedic doctors are equipped to handle a vast array of conditions affecting the musculoskeletal system. Here’s an overview of some common ailments they address:
- Fractures: Broken bones, ranging from simple hairline fractures to complex, multi-fragment fractures.
- Dislocations: When the ends of bones are forced out of their normal position in a joint.
- Sprains and Strains: Injuries to ligaments (sprains) and muscles or tendons (strains).
- Arthritis: A group of conditions that cause joint pain, swelling, and stiffness.
- Osteoporosis: A disease that weakens bones and makes them more likely to fracture.
- Back Pain: Pain in the back that can be caused by a variety of factors, including muscle strains, disc problems, and arthritis.
- Neck Pain: Pain in the neck that can be caused by similar factors as back pain.
- Sports Injuries: Injuries sustained during athletic activities, such as ACL tears, meniscus tears, and rotator cuff tears.
- Carpal Tunnel Syndrome: A condition that causes numbness, tingling, and pain in the hand and wrist.
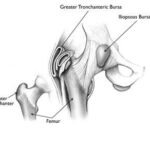
- Bursitis: Inflammation of a bursa, a fluid-filled sac that cushions joints.
- Tendonitis: Inflammation of a tendon, a cord that connects muscle to bone.
- Bone Tumors: Abnormal growths in bone tissue.
- Congenital Conditions: Conditions present at birth, such as scoliosis and clubfoot.
3.1. A Closer Look at Common Conditions
Let’s explore some of these conditions in more detail:
- Arthritis: This is a prevalent condition, especially among older adults. Osteoarthritis, the most common type, results from the breakdown of cartilage in joints. Rheumatoid arthritis is an autoimmune disease that causes inflammation of the joint lining.
- Fractures: These can occur due to trauma, such as falls or car accidents, or from overuse, such as stress fractures in athletes.
- Sports Injuries: These are common among athletes of all ages and skill levels. They can range from minor sprains and strains to severe ligament tears and fractures.
- Back Pain: This is a widespread problem that affects millions of people each year. It can be caused by a variety of factors, including poor posture, muscle strains, disc problems, and arthritis.
- Osteoporosis: This condition weakens bones and makes them more prone to fractures. It is more common in women after menopause.
3.2. How Bone Doctors Diagnose These Conditions
Orthopedic doctors use a variety of methods to diagnose musculoskeletal conditions, including:
- Physical Examination: A thorough assessment of the patient’s symptoms, medical history, and physical condition.
- Imaging Tests: X-rays, MRIs, CT scans, and other imaging tests to visualize bones, joints, and soft tissues.
- Nerve Conduction Studies: Tests to assess the function of nerves.
- Blood Tests: To help diagnose conditions such as rheumatoid arthritis and gout.
- Joint Aspiration: Removing fluid from a joint for analysis.
3.3. Treatment Options Available
The treatment options available for musculoskeletal conditions vary depending on the specific diagnosis and the severity of the condition. Some common treatments include:
- Medications: Pain relievers, anti-inflammatory drugs, and other medications to manage symptoms.
- Physical Therapy: Exercises and other therapies to improve strength, mobility, and function.
- Braces and Orthotics: Devices to support and protect injured or weakened bones and joints.
- Injections: Corticosteroid injections to reduce inflammation and pain.
- Surgery: Various surgical procedures to repair or replace damaged bones, joints, and soft tissues.
4. Exploring Other Types of Specialists
While orthopedic doctors are the primary “bone doctors,” other specialists also play a role in musculoskeletal health.
4.1. Rheumatologists
Rheumatologists specialize in the diagnosis and treatment of rheumatic diseases, which are conditions that affect the joints, muscles, and bones. Unlike orthopedists, who often focus on injuries and structural problems, rheumatologists typically treat autoimmune and inflammatory conditions.
Rheumatologists treat a wide variety of conditions, including:
- Rheumatoid Arthritis: An autoimmune disease that causes inflammation of the joint lining.
- Osteoarthritis: The most common type of arthritis, caused by the breakdown of cartilage in joints.
- Lupus: A chronic autoimmune disease that can affect joints, skin, kidneys, heart, lungs, blood vessels, and brain.
- Gout: A form of arthritis that causes sudden, severe attacks of pain and swelling in joints.
- Fibromyalgia: A condition that causes fatigue, muscle pain, and tenderness in joints.
- Osteoporosis: A disease that weakens bones and makes them more likely to fracture.
4.2. Osteopaths (Doctors of Osteopathic Medicine)
Osteopathic physicians (DOs) are licensed medical professionals who practice a “whole person” approach to medicine. They focus on the interconnectedness of the body’s systems and how they influence each other. Osteopaths use a variety of techniques to diagnose and treat musculoskeletal problems, including:
- Osteopathic Manipulative Treatment (OMT): A hands-on therapy that involves stretching, massaging, and moving joints to improve function and reduce pain.
- Medications: Prescription and over-the-counter medications to manage symptoms.
- Physical Therapy: Exercises and other therapies to improve strength, mobility, and function.
- Surgery: In some cases, osteopaths may perform surgery to address musculoskeletal problems.
4.3. Podiatrists
Podiatrists specialize in the diagnosis and treatment of foot and ankle problems. While they don’t treat the entire skeletal system, they are experts in the bones, joints, ligaments, tendons, and muscles of the foot and ankle.
Podiatrists treat a wide variety of conditions, including:
- Foot Pain: Pain in the foot that can be caused by a variety of factors, including plantar fasciitis, bunions, and hammertoe.
- Ankle Pain: Pain in the ankle that can be caused by sprains, strains, arthritis, and other conditions.
- Plantar Fasciitis: Inflammation of the plantar fascia, a thick band of tissue that runs along the bottom of the foot.
- Bunions: A bony bump that forms on the joint at the base of the big toe.
- Hammertoe: A deformity in which the toe is bent at the middle joint.
- Ingrown Toenails: When the edge of the toenail grows into the surrounding skin.
- Diabetic Foot Care: Specialized care for people with diabetes to prevent foot problems and complications.
4.4. Choosing the Right Specialist
Selecting the most appropriate specialist depends on your specific condition and symptoms. Here’s a general guideline:
| Specialist | Focus | Conditions Treated |
|---|---|---|
| Orthopedic Doctor | Injuries and structural problems of the musculoskeletal system | Fractures, dislocations, sprains, strains, arthritis, sports injuries |
| Rheumatologist | Autoimmune and inflammatory conditions affecting joints, muscles, bones | Rheumatoid arthritis, lupus, gout, fibromyalgia, osteoporosis |
| Osteopath | “Whole person” approach to musculoskeletal problems | Back pain, neck pain, joint pain, arthritis |
| Podiatrist | Foot and ankle problems | Foot pain, ankle pain, plantar fasciitis, bunions, hammertoe, ingrown toenails |
If you’re unsure which type of specialist to see, consult with your primary care physician. They can evaluate your symptoms and refer you to the most appropriate healthcare provider.
5. Staying Proactive With Bone Health
Maintaining strong and healthy bones is a lifelong endeavor. Implementing proactive measures can significantly reduce your risk of developing bone-related issues.
5.1. Nutrition for Bone Health
A balanced diet rich in essential nutrients is the foundation of bone health. Key nutrients include:
- Calcium: The primary building block of bone tissue. Good sources include dairy products, leafy green vegetables, and fortified foods. The National Osteoporosis Foundation recommends adults aged 19-50 consume 1,000 mg of calcium daily, while those over 50 should aim for 1,200 mg.
- Vitamin D: Essential for calcium absorption. Your body produces vitamin D when exposed to sunlight. Dietary sources include fatty fish, egg yolks, and fortified foods. The recommended daily intake for adults is 600 IU, increasing to 800 IU after age 70.
- Vitamin K: Plays a role in bone formation. Found in leafy green vegetables, broccoli, and Brussels sprouts.
- Magnesium: Contributes to bone strength and density. Found in nuts, seeds, whole grains, and leafy green vegetables.
- Phosphorus: Works with calcium to build strong bones. Found in dairy products, meat, poultry, fish, and eggs.
5.2. Exercise for Bone Strength
Weight-bearing exercises and resistance training are crucial for building and maintaining bone density. These activities stimulate bone cells and encourage them to produce new bone tissue.
- Weight-bearing exercises: Activities that force you to work against gravity, such as walking, running, dancing, and jumping.
- Resistance training: Exercises that use weights or resistance bands to strengthen muscles and bones. Examples include lifting weights, doing squats, and using resistance machines.
The American Bone Health organization recommends that adults engage in at least 30 minutes of weight-bearing exercise most days of the week, along with two to three sessions of resistance training per week.
5.3. Lifestyle Factors to Consider
Certain lifestyle choices can significantly impact bone health. It’s essential to:
- Quit smoking: Smoking weakens bones and increases the risk of fractures.
- Limit alcohol consumption: Excessive alcohol intake can interfere with calcium absorption and bone formation.
- Maintain a healthy weight: Being underweight or overweight can negatively affect bone health.
- Prevent falls: Falls are a major cause of fractures, especially in older adults. Take steps to reduce your risk of falling, such as wearing supportive shoes, using assistive devices, and making your home safe.
5.4. Regular Bone Density Screenings
Bone density screenings, also known as DEXA scans, measure the density of your bones and can help detect osteoporosis before a fracture occurs. The National Osteoporosis Foundation recommends that all women aged 65 and older undergo bone density screening. Younger women and men should also be screened if they have risk factors for osteoporosis.
These preventative measures can make a huge difference in the long run.
6. Cutting-Edge Advances in Bone Care
The field of orthopedic medicine is constantly evolving, with new technologies and treatments emerging regularly. Here are some of the latest advancements in bone care:
- Minimally Invasive Surgery: Surgical techniques that use small incisions and specialized instruments to minimize tissue damage and reduce recovery time.
- Robotic Surgery: The use of robotic systems to assist surgeons with complex procedures, improving precision and accuracy.
- 3D Printing: Creating customized implants and surgical guides using 3D printing technology.
- Biologic Therapies: Using the body’s own healing mechanisms to promote bone regeneration and repair.
- Regenerative Medicine: Developing new therapies that can regenerate damaged bone tissue.
- Computer-Assisted Surgery: Using computer software to plan and guide surgical procedures, improving accuracy and outcomes.
- Improved Implants: Development of new and improved implants for joint replacement and fracture fixation.
6.1. A Table of Recent Innovations
Here’s a quick look at some of the most promising recent innovations in bone care:
| Innovation | Description | Potential Benefits |
|---|---|---|
| Minimally Invasive Surgery | Small incisions, specialized instruments | Less pain, faster recovery, reduced risk of complications |
| Robotic Surgery | Robotic systems assist surgeons | Increased precision, improved accuracy, enhanced visualization |
| 3D Printing | Customized implants and surgical guides | Personalized treatment, improved fit, reduced surgical time |
| Biologic Therapies | Harnessing the body’s own healing mechanisms | Accelerated healing, reduced inflammation, improved bone regeneration |
| Regenerative Medicine | Therapies to regenerate damaged bone tissue | Potential to cure bone diseases and injuries, reduced need for surgery |
| Computer-Assisted Surgery | Software plans and guides surgery | Improved accuracy, better outcomes, reduced risk of complications |
| Improved Implants | Advanced materials and designs | Longer-lasting implants, improved function, reduced risk of failure |
6.2. How These Advances Benefit Patients
These advancements offer numerous benefits for patients, including:
- Reduced Pain: Minimally invasive techniques and improved pain management strategies can help reduce post-operative pain.
- Faster Recovery: Minimally invasive surgery and biologic therapies can shorten recovery times and allow patients to return to their normal activities sooner.
- Improved Outcomes: Robotic surgery and computer-assisted surgery can improve the accuracy and precision of surgical procedures, leading to better outcomes.
- Personalized Treatment: 3D printing and biologic therapies allow for customized treatment plans that are tailored to each patient’s individual needs.
- Less Invasive Procedures: Many of these advancements focus on less invasive approaches, reducing the need for open surgery and minimizing tissue damage.
6.3. The Future of Bone Care
The future of bone care is bright, with ongoing research and development focused on even more innovative technologies and treatments. Some areas of focus include:
- Stem Cell Therapy: Using stem cells to regenerate damaged bone tissue.
- Gene Therapy: Modifying genes to prevent or treat bone diseases.
- Nanotechnology: Developing nanoscale materials and devices to deliver drugs and therapies directly to bone cells.
- Artificial Intelligence: Using AI to diagnose bone diseases and plan surgical procedures.
- Wearable Sensors: Developing wearable sensors to monitor bone health and detect early signs of problems.
These advancements have the potential to revolutionize the way we care for our bones and joints, leading to improved outcomes and a better quality of life for millions of people.
7. Frequently Asked Questions (FAQ)
Here are some frequently asked questions about bone doctors and bone health:
-
What is the difference between an orthopedist and a chiropractor?
An orthopedist is a medical doctor who specializes in the musculoskeletal system and can diagnose and treat a wide range of bone and joint conditions. A chiropractor focuses on the alignment of the spine and uses manual adjustments to treat musculoskeletal problems.
-
Can a bone doctor treat arthritis?
Yes, orthopedic doctors and rheumatologists both treat arthritis. Orthopedists may focus on surgical interventions, while rheumatologists typically manage the condition with medication and other non-surgical treatments.
-
What is the best way to find a good bone doctor?
Ask your primary care physician for a referral, check online reviews, and verify the doctor’s credentials and experience.
-
How can I prepare for my first appointment with a bone doctor?
Gather your medical history, list your symptoms, bring any relevant imaging reports, and write down any questions you have.
-
What are the risks of bone surgery?
As with any surgery, there are risks involved, such as infection, bleeding, blood clots, and nerve damage. Your surgeon will discuss these risks with you before the procedure.
-
How long does it take to recover from a broken bone?
The recovery time varies depending on the severity of the fracture, the bone that is broken, and the individual’s overall health. It can take anywhere from a few weeks to several months.
-
Can I prevent osteoporosis?
Yes, you can reduce your risk of osteoporosis by eating a healthy diet, getting enough calcium and vitamin D, exercising regularly, and avoiding smoking and excessive alcohol consumption.
-
What is a bone density test?
A bone density test, also known as a DEXA scan, measures the density of your bones and can help detect osteoporosis before a fracture occurs.
-
Are there any natural remedies for bone pain?
Some natural remedies that may help with bone pain include turmeric, ginger, and omega-3 fatty acids. However, it’s important to consult with your doctor before trying any new remedies.
-
When should I see a doctor for bone pain?
See a doctor if you have persistent bone pain, limited range of motion, swelling, redness, or warmth around a joint, or difficulty performing daily activities.
8. Take Action for Your Bone Health Today
Understanding what a bone doctor is called and the conditions they treat is the first step towards better musculoskeletal health. Whether you’re dealing with a sports injury, chronic pain, or a degenerative condition, seeking professional help is essential.
At thebootdoctor.net, we’re dedicated to providing you with the information and resources you need to make informed decisions about your bone health. Explore our articles, guides, and expert advice to learn more about various conditions, treatment options, and preventative measures.
Ready to take the next step?
- Browse our extensive library of articles on foot and ankle health.
- Learn about common conditions and their treatments.
- Contact us with any questions or concerns.
Your feet are the foundation of your body, and we’re here to help you keep them strong and healthy. Let thebootdoctor.net be your trusted resource for all things foot and ankle related.
(Address: 6565 Fannin St, Houston, TX 77030, United States. Phone: +1 (713) 791-1414. Website: thebootdoctor.net.)