Describing pain to a doctor accurately is essential for effective diagnosis and treatment, and at thebootdoctor.net, we understand this. By clearly articulating the nature, location, and intensity of your pain, you empower your healthcare provider to tailor a personalized treatment plan that addresses your specific needs. Clear communication ensures you receive the most appropriate care, leading to quicker relief and improved quality of life. If you are looking for resources to help with foot pain, consider looking into therapeutic footwear, custom orthotics, or pain management strategies.
1. Why Accurately Describing Your Pain Matters
Accurately describing your pain is crucial because it guides your healthcare provider towards an accurate diagnosis and effective treatment plan. It’s like giving them the right map to navigate your health concerns.
1.1 Guiding Diagnosis
When you clearly describe your pain, you provide essential clues that help doctors pinpoint the underlying cause of your discomfort. Precise details about the location, type, and intensity of your pain act as breadcrumbs, leading healthcare providers closer to an accurate diagnosis. This targeted approach prevents misdiagnosis, saving you time and potential frustration.
1.2 Tailoring Treatment
The more detailed your description, the better your doctor can tailor a treatment plan to your unique needs. By understanding the specific characteristics of your pain, healthcare providers can select interventions that directly address the source of your discomfort. This personalized approach optimizes treatment outcomes, ensuring you receive the most effective care possible.
1.3 Avoiding Misdiagnosis
Inaccurate or vague descriptions can lead to misdiagnosis and inappropriate treatment. When doctors lack clear information about your pain, they may pursue avenues that don’t align with your actual condition, leading to unnecessary tests and ineffective interventions. Providing a precise account of your symptoms minimizes the risk of misdiagnosis, safeguarding your health and well-being.
1.4 Optimizing Communication
Describing your pain effectively enhances communication with your healthcare provider. It fosters a collaborative environment where you and your doctor can work together to understand your condition and develop a comprehensive treatment strategy. Open dialogue ensures your concerns are heard and addressed, promoting trust and confidence in your healthcare journey.
1.5 Enhancing Treatment Outcomes
Ultimately, accurately describing your pain contributes to better treatment outcomes. By equipping your healthcare provider with the information they need to make informed decisions, you increase the likelihood of receiving targeted interventions that alleviate your pain and improve your overall quality of life. This proactive approach empowers you to take control of your health and achieve lasting relief.
2. Key Aspects to Cover When Describing Pain
When describing pain to a doctor, covering key aspects such as location, intensity, type, duration, and aggravating factors ensures a comprehensive understanding. Providing specific details empowers healthcare professionals to accurately assess your condition and tailor an effective treatment plan.
2.1 Location
Pinpoint the exact area where you’re experiencing pain, whether it’s localized or radiating to other parts of your body. For example, if you have foot pain, specify whether it’s in the heel, arch, toes, or a combination of areas. Accurate localization helps healthcare providers narrow down potential causes and focus their examination.
2.2 Intensity
Use a pain scale, typically ranging from 0 to 10, to quantify the severity of your pain. A rating of 0 indicates no pain, while 10 represents the worst pain imaginable. Objectively assessing pain intensity provides a standardized measure for healthcare professionals to track changes in your condition over time.
2.3 Type
Describe the sensation of your pain using descriptive terms such as sharp, dull, throbbing, burning, stabbing, or aching. Each adjective provides valuable insights into the underlying pathology. For instance, sharp pain may suggest nerve involvement, while dull pain may indicate muscle strain or inflammation.
2.4 Duration
Indicate how long you’ve been experiencing the pain, whether it’s constant, intermittent, or episodic. Knowing the duration helps healthcare providers differentiate between acute and chronic conditions. Acute pain typically arises suddenly and resolves within a short period, while chronic pain persists for several months or longer.
2.5 Aggravating and Alleviating Factors
Identify activities, positions, or movements that worsen or relieve your pain. For example, does walking exacerbate your foot pain, or does rest provide relief? Understanding these factors helps healthcare providers identify triggers and tailor recommendations to minimize discomfort.
2.6 Associated Symptoms
Mention any accompanying symptoms, such as swelling, stiffness, numbness, tingling, weakness, or changes in skin color. These additional details can provide clues about the underlying cause of your pain. For instance, swelling and redness may indicate inflammation or infection, while numbness and tingling may suggest nerve compression.
 Foot Pain Area
Foot Pain Area
2.7 Impact on Daily Activities
Explain how the pain affects your ability to perform daily tasks, such as walking, standing, sleeping, or working. Describing the functional limitations imposed by your pain helps healthcare providers assess the severity of your condition and prioritize appropriate interventions. For example, if foot pain prevents you from walking without assistance, it may warrant more aggressive treatment.
3. Using Descriptive Language to Explain Your Pain
Using descriptive language to explain your pain involves employing vivid adjectives and analogies to convey the specific characteristics of your discomfort. By painting a detailed picture with words, you enable healthcare professionals to better understand your experience and tailor their approach accordingly.
3.1 Specific Adjectives
Utilize specific adjectives to characterize the nature of your pain. Instead of simply saying “it hurts,” try to elaborate on the sensation you’re experiencing. For instance, you might describe the pain as “sharp and stabbing,” “dull and aching,” “burning and tingling,” or “throbbing and pounding.” Each adjective provides valuable insight into the underlying pathology.
3.2 Analogies
Employ analogies to convey the intensity or quality of your pain in relatable terms. For example, you might say the pain feels like “a knife twisting in my joint,” “a tight band squeezing my head,” or “an electric shock shooting down my leg.” Analogies help healthcare professionals grasp the subjective nature of your pain by comparing it to familiar sensations.
3.3 Sensory Details
Incorporate sensory details to describe how the pain affects your senses. Does the pain make your skin feel hot or cold? Does it cause tingling or numbness? Does it make you feel dizzy or nauseous? Sensory details add depth to your description and provide additional clues about the underlying cause of your discomfort.
3.4 Comparisons
Compare your current pain to past experiences to provide context and perspective. Have you ever felt this type of pain before? If so, how does it compare in terms of intensity, duration, and quality? Comparing your current pain to previous episodes can help healthcare professionals differentiate between new and recurring conditions.
3.5 Emotional Impact
Discuss the emotional impact of your pain on your mood, behavior, and overall well-being. Does the pain make you feel anxious, depressed, irritable, or hopeless? Does it interfere with your ability to work, socialize, or enjoy hobbies? Addressing the emotional aspects of pain can help healthcare professionals develop a comprehensive treatment plan that addresses both the physical and psychological dimensions of your condition.
3.6 Examples of Descriptive Phrases
Here are some examples of descriptive phrases you can use to explain your pain:
- “The pain feels like a throbbing ache deep inside my foot, like a constant pressure that won’t go away.”
- “It’s a sharp, stabbing pain that shoots up my leg whenever I put weight on it, like stepping on broken glass.”
- “The pain is a burning sensation that radiates from my toes to my heel, like my foot is on fire.”
- “It’s a dull, aching pain that’s always there, but it gets worse when I walk or stand for long periods, like a heavy weight pulling my foot down.”
- “The pain is like pins and needles, a tingling sensation that makes my foot feel numb and weak.”
By using descriptive language to explain your pain, you can provide healthcare professionals with a clearer understanding of your experience and facilitate more effective diagnosis and treatment.
4. Common Mistakes to Avoid When Describing Pain
When describing pain, avoid vague language, exaggeration, minimizing the pain, focusing solely on intensity, and neglecting emotional aspects. Clear, accurate communication ensures proper assessment and effective treatment.
4.1 Using Vague Language
Avoid using vague terms like “it hurts” or “it’s uncomfortable” without providing specific details about the location, intensity, or type of pain. Instead, use descriptive language to convey the sensation you’re experiencing, such as “sharp,” “dull,” “throbbing,” or “burning.”
4.2 Exaggerating the Pain
Refrain from exaggerating the severity of your pain, as it can undermine your credibility and lead to misdiagnosis. Provide an honest assessment of your pain level based on your own perception and experience.
4.3 Minimizing the Pain
Conversely, avoid downplaying the significance of your pain, especially if it’s significantly impacting your daily life. Accurately representing the extent of your discomfort ensures that healthcare professionals take your concerns seriously and provide appropriate treatment.
4.4 Focusing Solely on Intensity
While intensity is an important aspect of pain assessment, it’s essential to consider other factors, such as the location, type, duration, and aggravating factors. Providing a comprehensive description of your pain allows healthcare professionals to gain a holistic understanding of your condition.
4.5 Neglecting Emotional Aspects
Don’t overlook the emotional impact of your pain on your mood, behavior, and overall well-being. Pain can often be accompanied by feelings of anxiety, depression, frustration, or hopelessness. Addressing these emotional aspects can help healthcare professionals develop a comprehensive treatment plan that addresses both the physical and psychological dimensions of your condition.
4.6 Failing to Mention Relevant History
Omit relevant medical history, such as previous injuries, surgeries, or chronic conditions, can hinder accurate diagnosis and treatment. Provide a thorough account of your medical background, including any factors that may be contributing to your current pain.
4.7 Not Asking Questions
Hesitate to ask questions or seek clarification about your condition or treatment options. Engage actively in the conversation with your healthcare provider to ensure you understand the diagnosis, prognosis, and management plan.
By avoiding these common mistakes when describing pain, you can facilitate more effective communication with healthcare professionals and optimize your chances of receiving appropriate and timely care.
5. Tools and Scales to Help Describe Pain
Tools and scales like the Numeric Rating Scale (NRS), Visual Analog Scale (VAS), and McGill Pain Questionnaire can assist in describing pain. These resources offer standardized methods for quantifying and characterizing pain, facilitating communication between patients and healthcare providers.
5.1 Numeric Rating Scale (NRS)
The Numeric Rating Scale (NRS) is a simple and widely used tool that asks patients to rate their pain on a scale from 0 to 10, where 0 represents “no pain” and 10 represents “the worst pain imaginable.” Patients select the number that best reflects their current level of pain intensity. The NRS provides a quick and straightforward way to quantify pain and track changes over time.
5.2 Visual Analog Scale (VAS)
The Visual Analog Scale (VAS) consists of a 10-centimeter line with endpoints labeled “no pain” and “worst pain imaginable.” Patients mark a point on the line that corresponds to their current level of pain intensity. The distance from the “no pain” end of the line to the patient’s mark is measured to determine the pain score. The VAS offers a continuous measure of pain intensity, allowing for more subtle gradations than the NRS.
5.3 McGill Pain Questionnaire
The McGill Pain Questionnaire is a comprehensive tool that assesses multiple dimensions of pain, including sensory, affective, and evaluative aspects. It consists of a series of words and phrases that describe different qualities of pain, such as throbbing, shooting, burning, aching, and tender. Patients select the words that best describe their pain experience. The McGill Pain Questionnaire provides a detailed profile of pain characteristics, helping healthcare providers gain a deeper understanding of the patient’s condition.
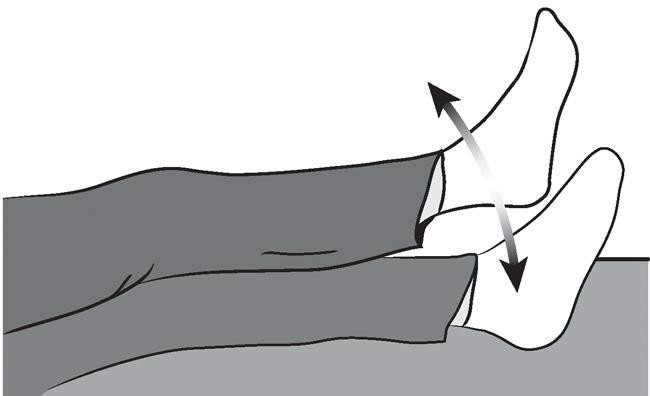
5.4 Pain Drawings
Pain drawings involve asking patients to shade or mark areas on a body diagram where they are experiencing pain. Patients may also be asked to indicate the type of pain they are feeling in different areas, such as sharp, dull, or radiating. Pain drawings can help healthcare providers visualize the location and distribution of pain, as well as identify patterns that may suggest underlying pathology.
5.5 Wong-Baker Faces Pain Rating Scale
The Wong-Baker Faces Pain Rating Scale is a visual tool designed for children and individuals who may have difficulty expressing their pain verbally. It consists of a series of faces depicting different levels of pain intensity, ranging from a smiling face representing “no pain” to a crying face representing “the worst pain.” Patients select the face that best reflects their current level of pain. The Wong-Baker Faces Pain Rating Scale provides a simple and accessible way to assess pain in diverse populations.
5.6 Choosing the Right Tool
The choice of which pain assessment tool to use depends on various factors, including the patient’s age, cognitive abilities, language proficiency, and the specific goals of the assessment. Healthcare providers should select a tool that is appropriate for the individual patient and that provides meaningful information to guide diagnosis and treatment.
By utilizing these tools and scales, patients and healthcare providers can enhance communication about pain and facilitate more effective management strategies.
:max_bytes(150000):strip_icc():format(webp)/how-to-use-the-pain-scale-2564677-v2-9817c15b970a43329079818b4ca782a2.png)
6. Preparing for Your Doctor’s Appointment
Preparing for your doctor’s appointment involves gathering relevant information, documenting your symptoms, and formulating questions. Thorough preparation ensures efficient communication and maximizes the effectiveness of your consultation.
6.1 Gathering Relevant Information
Before your appointment, gather relevant information about your medical history, including any previous illnesses, surgeries, allergies, and medications you’re currently taking. Also, collect any records or test results related to your current condition, such as X-rays, MRIs, or blood work. Having this information readily available can help your doctor gain a comprehensive understanding of your health status and identify potential factors contributing to your pain.
6.2 Documenting Your Symptoms
Keep a detailed record of your symptoms, including when they started, how they’ve changed over time, and any factors that seem to trigger or alleviate them. Document the location, intensity, type, and duration of your pain, as well as any associated symptoms such as swelling, stiffness, numbness, or tingling. Use a pain scale to rate the severity of your pain at different times of the day or during various activities. Accurate documentation can provide valuable insights for your doctor and help them track your progress over time.
6.3 Formulating Questions
Prepare a list of questions you want to ask your doctor during the appointment. These questions may relate to the cause of your pain, potential treatment options, lifestyle modifications, or strategies for managing your symptoms at home. Prioritize your questions based on their importance and relevance to your concerns. Asking thoughtful questions demonstrates your engagement in your healthcare and ensures that you receive the information you need to make informed decisions.
6.4 Bringing a Support Person
Consider bringing a trusted friend or family member to your appointment to provide support, take notes, and help you remember important details. A support person can serve as an extra set of ears and eyes, ensuring that you don’t miss any crucial information or instructions from your doctor. They can also offer emotional support and encouragement during what may be a stressful or overwhelming experience.
6.5 Arriving on Time
Arrive at your doctor’s office on time or even a few minutes early to allow yourself time to check in, complete any necessary paperwork, and relax before your appointment. Arriving late may shorten the amount of time you have with your doctor and prevent you from addressing all of your concerns.
6.6 Being Open and Honest
Be open and honest with your doctor about your symptoms, concerns, and lifestyle habits. Withholding information or providing inaccurate details can hinder their ability to accurately diagnose and treat your condition. Trust your doctor to provide you with the best possible care, and work together as a team to achieve your health goals.
By preparing thoroughly for your doctor’s appointment, you can ensure that you get the most out of your consultation and receive the care and attention you deserve.
7. Understanding Different Types of Pain
Understanding different types of pain, such as nociceptive, neuropathic, and inflammatory pain, is essential for effective diagnosis and treatment. Each type arises from distinct mechanisms and requires tailored management strategies.
7.1 Nociceptive Pain
Nociceptive pain is caused by activation of nociceptors, which are specialized sensory receptors that detect tissue damage. It typically results from injuries such as cuts, burns, fractures, or sprains. Nociceptive pain is often described as sharp, aching, throbbing, or pressure-like. It is usually localized to the site of injury and tends to worsen with movement or pressure.
7.2 Neuropathic Pain
Neuropathic pain arises from damage or dysfunction of the nervous system, including the peripheral nerves, spinal cord, or brain. It can result from conditions such as diabetes, shingles, multiple sclerosis, or nerve compression. Neuropathic pain is often described as burning, shooting, stabbing, or electric shock-like. It may be accompanied by numbness, tingling, or sensitivity to touch.
7.3 Inflammatory Pain
Inflammatory pain is caused by inflammation in the body, which can occur in response to injury, infection, or autoimmune disorders. Inflammation triggers the release of chemicals that sensitize nerve endings and amplify pain signals. Inflammatory pain is often described as aching, throbbing, or tenderness. It may be associated with swelling, redness, and warmth in the affected area.
7.4 Psychogenic Pain
Psychogenic pain, also known as psychological pain, is pain that is believed to be caused, increased, or prolonged by mental, emotional, or behavioral factors. Headache, muscle pain, back pain, and stomach pain are some of the most common types of psychogenic pain.
7.5 Radicular Pain
Radicular pain is pain that radiates along the course of a nerve, typically due to compression or irritation of a nerve root in the spine. It is often described as shooting, burning, or electric shock-like. Radicular pain may be accompanied by numbness, tingling, or weakness in the affected limb.
7.6 Referred Pain
Referred pain is pain that is felt in a location different from where the actual injury or problem exists. This occurs because nerves from different parts of the body converge on the same pathways in the spinal cord. Referred pain is often described as dull, aching, or diffuse.
7.7 Breakthrough Pain
Breakthrough pain is a sudden flare-up of pain that occurs despite regular use of pain medication. It is often unpredictable and can be severe. Breakthrough pain is common in individuals with chronic pain conditions, such as cancer or arthritis.
By understanding these different types of pain, healthcare providers can better assess the underlying causes of pain and develop targeted treatment strategies to alleviate discomfort and improve quality of life.
8. Questions Your Doctor Might Ask About Your Pain
Your doctor might ask questions about the onset, location, intensity, type, duration, aggravating factors, alleviating factors, associated symptoms, impact on daily activities, and medical history related to your pain. Answering these questions comprehensively aids in accurate diagnosis and effective treatment planning.
8.1 When Did the Pain Start?
Understanding the onset of your pain helps determine whether it’s acute (sudden and recent) or chronic (long-lasting).
8.2 Where Exactly Is the Pain Located?
Pinpointing the precise location of your pain is crucial for identifying the underlying cause and potential sources of discomfort.
8.3 How Intense Is the Pain on a Scale of 0 to 10?
Using a pain scale provides a standardized way to quantify the severity of your pain and track changes over time.
8.4 What Does the Pain Feel Like?
Describing the sensation of your pain using descriptive terms such as sharp, dull, throbbing, burning, stabbing, or aching provides valuable insights into the underlying pathology.
8.5 How Long Does the Pain Last?
Knowing the duration of your pain helps differentiate between acute and chronic conditions and assess its impact on your daily life.
8.6 What Makes the Pain Worse?
Identifying activities, positions, or movements that exacerbate your pain helps pinpoint triggers and guide recommendations for avoiding discomfort.
8.7 What Makes the Pain Better?
Understanding factors that alleviate your pain, such as rest, medication, or specific therapies, provides insights into potential management strategies.
8.8 Are There Any Other Symptoms Associated With the Pain?
Mentioning accompanying symptoms such as swelling, stiffness, numbness, tingling, weakness, or changes in skin color provides additional clues about the underlying cause of your pain.
8.9 How Does the Pain Affect Your Daily Activities?
Explaining how the pain impacts your ability to perform daily tasks such as walking, standing, sleeping, or working helps assess the severity of your condition and prioritize appropriate interventions.
8.10 What Is Your Medical History?
Providing a thorough account of your medical background, including previous injuries, surgeries, chronic conditions, and medications, helps identify potential factors contributing to your current pain.
8.11 Have You Tried Any Treatments for the Pain?
Describing any treatments you’ve already tried, whether over-the-counter medications, home remedies, or professional therapies, helps healthcare providers understand what has worked or not worked in the past and tailor their approach accordingly.
By anticipating these questions and preparing comprehensive answers, you can facilitate a more productive conversation with your doctor and ensure that they have the information they need to accurately diagnose and effectively treat your pain.
9. The Role of Imaging and Tests in Diagnosing Pain
Imaging and tests play a crucial role in diagnosing pain by providing healthcare professionals with visual and objective information about the underlying structures and functions of the body. These diagnostic tools help identify abnormalities, rule out potential causes of pain, and guide treatment decisions.
9.1 X-Rays
X-rays use electromagnetic radiation to create images of bones and dense tissues. They are commonly used to detect fractures, dislocations, arthritis, and other structural abnormalities. X-rays are quick, non-invasive, and relatively inexpensive, making them a valuable tool for initial evaluation of musculoskeletal pain.
9.2 Magnetic Resonance Imaging (MRI)
MRI uses magnetic fields and radio waves to produce detailed images of soft tissues such as muscles, ligaments, tendons, nerves, and spinal cord. MRI is particularly useful for diagnosing conditions such as herniated discs, nerve compression, soft tissue injuries, and tumors. It provides excellent visualization of anatomical structures and can detect subtle abnormalities that may not be visible on X-rays.
9.3 Computed Tomography (CT) Scans
CT scans use X-rays to create cross-sectional images of the body. They provide more detailed information than traditional X-rays and can be used to evaluate bones, soft tissues, and blood vessels. CT scans are often used to diagnose conditions such as fractures, infections, tumors, and internal injuries.
9.4 Ultrasound
Ultrasound uses high-frequency sound waves to create real-time images of soft tissues such as muscles, tendons, ligaments, and blood vessels. It is non-invasive, painless, and does not involve radiation. Ultrasound is commonly used to diagnose conditions such as tendonitis, bursitis, muscle strains, and blood clots.
9.5 Nerve Conduction Studies (NCS) and Electromyography (EMG)
NCS and EMG are tests that assess the function of nerves and muscles. NCS measures the speed at which electrical impulses travel along nerves, while EMG measures the electrical activity of muscles. These tests are used to diagnose conditions such as nerve damage, nerve compression, and muscle disorders.
9.6 Blood Tests
Blood tests can help identify underlying medical conditions that may be contributing to pain, such as infections, inflammation, autoimmune disorders, or metabolic abnormalities. Common blood tests used in the evaluation of pain include complete blood count (CBC), erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), and rheumatoid factor (RF).
9.7 Diagnostic Injections
Diagnostic injections involve injecting local anesthetic or corticosteroids into specific areas to determine the source of pain. For example, injections into joints, nerves, or muscles can help identify whether these structures are contributing to the patient’s symptoms.
9.8 Interpreting Results
The results of imaging and tests are interpreted by healthcare professionals, such as radiologists, neurologists, or orthopedic surgeons, who have specialized training in these areas. They analyze the images and data to identify abnormalities, rule out potential causes of pain, and guide treatment decisions.
By utilizing imaging and tests appropriately, healthcare professionals can gain valuable insights into the underlying causes of pain and develop targeted treatment strategies to alleviate discomfort and improve quality of life.
10. Treatment Options Based on Pain Description
Treatment options vary depending on the pain description and underlying cause, ranging from medication and physical therapy to injections and surgery. Tailoring treatment to the specific characteristics of pain ensures the most effective and personalized approach.
10.1 Medication
Medications play a crucial role in managing pain and can be tailored to the specific type and intensity of pain experienced. Over-the-counter pain relievers such as acetaminophen and nonsteroidal anti-inflammatory drugs (NSAIDs) can help alleviate mild to moderate pain. Prescription medications, such as opioids, may be necessary for more severe pain, but they should be used with caution due to the risk of side effects and dependence.
10.2 Physical Therapy
Physical therapy involves exercises, stretches, and manual therapies designed to improve strength, flexibility, and range of motion. It can be beneficial for managing musculoskeletal pain, such as back pain, neck pain, and joint pain. Physical therapists can also teach patients techniques for managing pain at home, such as proper posture, body mechanics, and ergonomic adjustments.
10.3 Injections
Injections can be used to deliver medication directly to the site of pain. Corticosteroid injections can reduce inflammation and relieve pain in joints, muscles, and nerves. Nerve blocks can temporarily block pain signals from specific nerves. Trigger point injections can relieve muscle pain and spasm.
10.4 Surgery
Surgery may be necessary to correct structural abnormalities or relieve nerve compression that is causing pain. Surgical options vary depending on the underlying cause of pain and may include joint replacement, spinal fusion, nerve decompression, or tumor removal.
10.5 Alternative Therapies
Alternative therapies such as acupuncture, massage therapy, chiropractic care, and yoga may provide relief from certain types of pain. These therapies can help reduce muscle tension, improve circulation, and promote relaxation.
10.6 Lifestyle Modifications
Lifestyle modifications such as regular exercise, weight management, stress reduction, and smoking cessation can help improve overall health and reduce pain. Maintaining a healthy lifestyle can also help prevent future pain problems.
10.7 Psychological Therapies
Psychological therapies such as cognitive-behavioral therapy (CBT) and mindfulness-based stress reduction (MBSR) can help patients cope with chronic pain by changing negative thought patterns and promoting relaxation. These therapies can also help patients develop coping skills for managing pain flare-ups and improving overall quality of life.
By considering the pain description and underlying cause, healthcare professionals can develop individualized treatment plans that address the specific needs of each patient. Effective pain management requires a multidisciplinary approach that combines medication, physical therapy, lifestyle modifications, and psychological therapies to provide comprehensive relief and improve overall well-being.
Effective communication is key when describing pain to your doctor. The more information you can provide, the better equipped they will be to diagnose and treat the root cause of your discomfort. Remember to be specific, use descriptive language, and don’t hesitate to ask questions.
At thebootdoctor.net, we understand the importance of accurate information when it comes to your foot health. Visit our website to explore a wealth of articles, guides, and resources designed to help you understand your condition and find the best path to recovery. Our team of experts is dedicated to providing you with the knowledge and support you need to keep your feet healthy and happy.
Do you have foot pain that is keeping you from enjoying your active lifestyle? Contact us today for a consultation or to schedule an appointment. Address: 6565 Fannin St, Houston, TX 77030, United States. Phone: +1 (713) 791-1414. Website: thebootdoctor.net.
Frequently Asked Questions (FAQs)
1. What if I can’t pinpoint the exact location of my pain?
If you can’t pinpoint the exact location, describe the general area and any patterns of radiation. For example, “It’s mostly in my lower back, but sometimes it shoots down my leg.”
2. How do I describe pain that comes and goes?
Describe the frequency, duration, and intensity of the pain episodes. Note any triggers or patterns you’ve noticed.
3. Is it okay to use a pain scale even if my pain is mild?
Yes, using a pain scale helps quantify even mild pain, providing a baseline for comparison over time.
4. Should I mention over-the-counter medications I’ve tried?
Absolutely. Inform your doctor about any medications, supplements, or home remedies you’ve used and their effects.
5. What if I’m worried about being perceived as a complainer?
Focus on accurately describing your symptoms and their impact on your daily life. Your doctor is there to help you.
6. Can emotional distress affect how I perceive pain?
Yes, stress, anxiety, and depression can amplify pain. Mention any emotional factors that may be contributing to your experience.
7. How important is it to mention past injuries or surgeries?
Very important. Past injuries or surgeries can provide valuable clues about the potential cause of your pain.
8. What if I don’t know the medical terms to describe my pain?
Use simple, descriptive language that accurately conveys your sensations. Your doctor can help translate if needed.
9. Should I bring a list of questions to my appointment?
Yes, preparing a list of questions ensures you address all your concerns and get the information you need.
10. What if I feel like my doctor isn’t taking my pain seriously?
Consider seeking a second opinion from another healthcare provider who is more attentive to your concerns.
Remember, your pain experience is unique, and effective communication is essential for accurate diagnosis and appropriate treatment.
