 Woman downplaying her arthritis pain
Woman downplaying her arthritis pain
It’s a common scenario: you’re in the doctor’s office, and when asked about your pain or arthritis symptoms, you find yourself minimizing them. Perhaps you shrug it off with a “it’s not too bad” or “I can manage.” If this sounds familiar, you’re not alone. Many individuals with chronic conditions, including osteoarthritis and other forms of arthritis, admit to downplaying their symptoms.
Members of the CreakyJoints community have openly discussed this tendency. Anne M. commented, “If I didn’t downplay my pain I wouldn’t talk about anything else! Boring!” Becka L. echoed this sentiment, explaining she downplays symptoms to avoid bothering others: “I don’t annoy people because everyone is like ‘you’re only 36’ and they get sick of the complaints. So I walk around and act normal if possible but my ankles, knees, and hips really hurt.”
While downplaying symptoms might be a coping mechanism in social situations, it becomes problematic when this habit extends to your medical appointments. The one place where honesty is paramount, and downplaying can be detrimental, is in your doctor’s office. But could this tendency to minimize your experience actually make conditions like osteoarthritis worse? Emerging research and expert opinions suggest the answer is a resounding yes.
Why We Downplay Symptoms to Doctors: Unpacking the Reasons
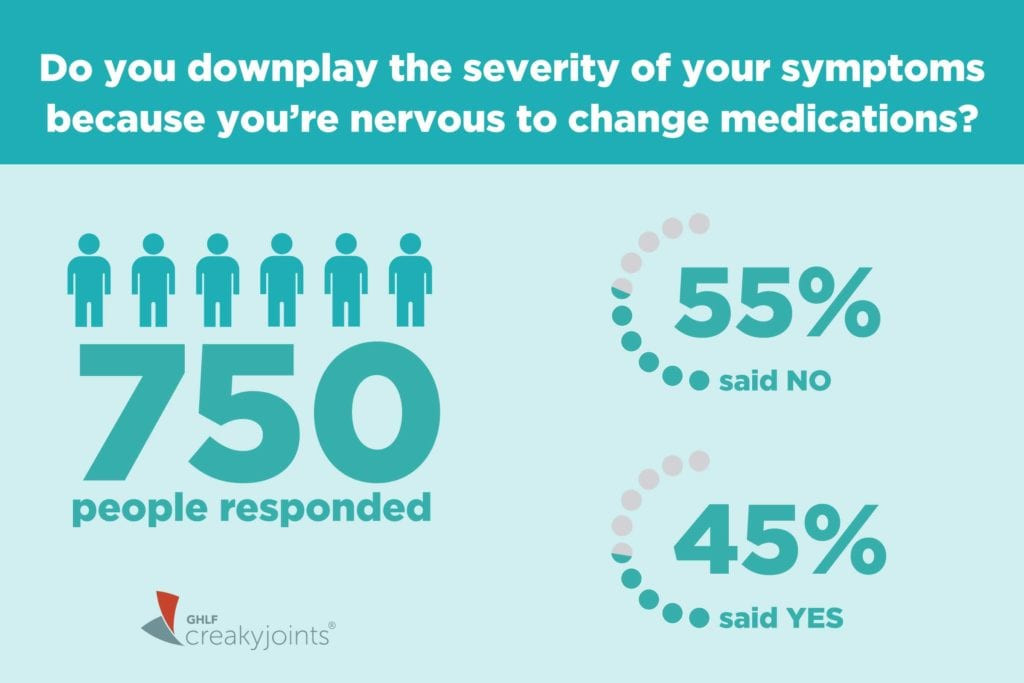
A recent ArthritisPower Community Poll shed light on this issue, revealing that a significant portion of patients downplay symptom severity specifically due to concerns about medication changes. Out of 750 respondents, 45 percent admitted to minimizing their symptoms because they were nervous about potential medication adjustments. This highlights a crucial barrier to effective communication and treatment.
According to Dr. Doug Roberts, a rheumatologist and founder of PainSpot.com, several underlying reasons contribute to patients downplaying their symptoms. Understanding these reasons is the first step in overcoming this counterproductive habit.
“It’s Good Enough”: Accepting Unnecessary Suffering
One prevalent thought pattern is accepting a certain level of pain and discomfort as an inevitable part of living with a chronic condition like osteoarthritis. Patients might compare their current state to their condition at diagnosis, thinking, “I’m doing much better than before.” While acknowledging progress is positive, settling for “good enough” when you could feel significantly better is not.
Dr. Roberts notes this resilience in patients, stating, “RA patients are a tough bunch. They learn to tolerate symptoms.” However, tolerating symptoms, especially in inflammatory conditions, can have far-reaching consequences beyond just joint pain. Inflammatory arthritis, including some types of osteoarthritis, affects the entire body, increasing the risk of comorbidities like heart disease and certain cancers. Ignoring persistent symptoms means ignoring potential systemic inflammation and its associated risks. Adjusting your lifestyle to accommodate pain, such as using mobility aids or limiting activities, is a form of downplaying if it masks the true severity of your condition from your doctor.
Fear of Complaining or Imposing: The Burden Mentality
Another significant barrier is the fear of being perceived as a complainer or burdening the doctor. Patients often hesitate to fully express their symptoms, worrying they might sound like they are “whining, imposing, or overreacting,” as explained by rheumatologist Dr. Ashira Blazer from NYU Langone Health. This reluctance stems from the difficulty in discerning what constitutes a “serious” symptom versus a minor discomfort.
However, medical professionals emphasize that sharing your experiences is not complaining; it’s providing essential data for effective diagnosis and treatment. Dr. Roberts stresses, “I don’t see it as complaining. The information you give me is just data that I use to help you. It gives me the best chance of helping you feel better.” Doctors rely on patient input to understand the full clinical picture, and withholding information hinders their ability to provide optimal care. It’s the doctor’s responsibility to assess symptom significance, and your responsibility to communicate them honestly and completely.
Avoiding the Unknowns of New Treatments: Fear of Change
The apprehension surrounding medication changes is a major driver of symptom downplaying. The prospect of new side effects, insurance complications, or altered medication routines can be daunting. Change, especially in healthcare, can feel scary and uncertain.
It’s important to remember that reporting new or worsening symptoms doesn’t automatically trigger a medication overhaul. Dr. Blazer clarifies, “More often than not, I don’t change medication when people report a new symptom or pain.” Doctors utilize a comprehensive approach, considering self-reported symptoms alongside bloodwork, imaging, physical exams, and quality-of-life assessments to determine if treatment adjustments are necessary. Shared decision-making is key, with doctors and patients collaborating on treatment plans.
Furthermore, understanding the context of potential side effects can alleviate anxiety. Dr. Roberts advises asking doctors to contextualize risks, using infection risk percentages as an example to illustrate that side effects are not guaranteed. It’s also crucial to weigh the risks of medication against the risks of uncontrolled disease progression. As Dr. Blazer points out, “medications have side effects, but diseases have effects… No medication would be approved if it were more dangerous than having the disease itself.” Untreated or poorly managed osteoarthritis can lead to significant joint damage and functional decline over time.
The Fear of the Diagnosis: Preferring Not to Know
Sometimes, downplaying symptoms stems from a deeper fear – the fear of what those symptoms might signify. Facing the unknown can be overwhelming, and a natural reaction is to avoid seeking information, hoping the problem will resolve itself. This “ostrich effect” – sticking your head in the sand – can lead to prolonged suffering and delayed diagnosis.
Catastrophizing is common when faced with health uncertainties, but often, the reality is less frightening than imagined fears. Dr. Blazer emphasizes, “You might be thinking the worst, but your symptoms might be easily explained by your physician.” She provides the example of patients enduring hip pain for weeks, fearing hip replacement, only to be diagnosed with trochanteric bursitis, a common condition unrelated to osteoarthritis, treatable with conservative measures.
Similarly, the story of RA patient Patty Deters illustrates this point. Experiencing a flare-up after remission, she feared her RA was worsening, but it turned out to be tendinitis from overuse. Knowing the actual cause, even if it requires treatment, is often less distressing than living with uncertainty and unaddressed symptoms. “A lot of times there is comfort in knowing whatever you have,” Dr. Blazer concludes. “There can be more suffering when you don’t know what’s wrong.”
The Real Impact: How Downplaying Symptoms Worsens Osteoarthritis and Overall Health
Downplaying symptoms, while seemingly a minor act of self-preservation or social grace, can have significant negative consequences, particularly for progressive conditions like osteoarthritis. By not accurately conveying the severity and nature of your symptoms, you hinder your doctor’s ability to:
- Accurately assess disease activity: Osteoarthritis management relies on understanding the current level of pain, stiffness, and functional limitations. Downplayed symptoms skew this assessment.
- Make informed treatment decisions: Treatment escalations or adjustments are often based on symptom reports. Minimized symptoms may lead to undertreatment and disease progression.
- Monitor treatment effectiveness: If you downplay ongoing symptoms, it becomes difficult to determine if your current treatment regimen is truly working or if modifications are needed.
- Identify and address comorbidities: As mentioned, inflammatory conditions, and even osteoarthritis to some extent, can increase the risk of other health problems. Downplaying symptoms can delay the recognition and management of these related conditions.
Ultimately, downplaying symptoms can lead to delayed or inadequate treatment, resulting in:
- Increased joint damage: In osteoarthritis, persistent symptoms can indicate ongoing cartilage breakdown and joint deterioration. Untreated, this damage can worsen over time, leading to more significant pain and disability.
- Reduced quality of life: Uncontrolled pain and functional limitations directly impact daily life, affecting mobility, sleep, mood, and overall well-being.
- Progression of osteoarthritis: While osteoarthritis isn’t always inflammatory, pain and limited mobility can contribute to muscle weakness, further joint stress, and a cycle of worsening symptoms.
- Increased risk of comorbidities: Systemic inflammation, even in some forms of osteoarthritis, can contribute to cardiovascular disease and other health issues if not properly managed.
Speak Up for Better Health: The Importance of Honest Communication
Getting your osteoarthritis, or any chronic condition, under control is paramount for protecting your long-term health and well-being. This often involves open and honest communication with your healthcare provider. Remember, doctors are partners in your health journey, and accurate information is their most valuable tool.
A study from the ArthritisPower research registry highlighted a concerning trend: only 37 percent of rheumatoid arthritis patients with high disease activity were offered a treatment change at their last visit. This suggests a potential gap in communication and proactive treatment adjustments. W. Benjamin Nowell, PhD, director of Patient-Centered Research at the Global Healthy Living Foundation, emphasizes the need for patient empowerment: “This study suggests that people living with RA need to feel empowered to discuss and consider treatment escalation with their doctor when both agree that a change is merited.”
With an expanding array of treatment options available for arthritis, including osteoarthritis, there is no reason to silently endure symptoms. Dr. Blazer encourages proactive communication: “It doesn’t make sense to ignore symptoms, because there are always more options.” Honest and open dialogue ensures you receive the best possible care, leading to better symptom management, improved quality of life, and potentially slowing the progression of osteoarthritis and protecting your overall health. Don’t let the reasons for downplaying symptoms become barriers to effective treatment. Speak openly, be honest, and prioritize your health.
