The doctor’s white coat is arguably one of the most recognizable pieces of professional attire in the world, instantly evoking images of healing, expertise, and trust. Steeped in history and symbolism, this garment has become synonymous with the medical profession. But beyond its iconic status, the white coat is also a subject of ongoing debate. Is it a powerful symbol of professionalism and patient care, or an outdated relic that poses hygiene risks and reinforces hierarchical structures within medicine?
A Garment Rooted in History and Symbolism
The adoption of the white coat by doctors in the late 19th century marked a significant shift in medical practice. Prior to this period, black coats were the norm, associating physicians with scholarly pursuits and the somber nature of illness and mortality. The transition to white was deliberate and symbolic. It was during this era that evidence-based medicine began to take hold, and the white coat was embraced to visually distinguish scientifically-minded physicians from the dubious practices of “quacks and snake-oil healers.” White, representing purity, cleanliness, and scientific rigor, became the color of modern medicine.
Today, the symbolism of the white coat remains potent, though interpretations vary. For many, it embodies the core values of the medical profession: professionalism, integrity, and a deep commitment to patient well-being. The white coat ceremony, a rite of passage in 97% of medical schools, further reinforces this symbolism, welcoming aspiring doctors into the medical community and imbuing them with the responsibilities associated with the profession.
However, the white coat’s symbolism is not universally positive. Some perceive it as a symbol of elitism, creating a barrier between doctors and patients. Furthermore, growing concerns about hygiene and infection control have cast a shadow on the once pristine image of the white coat, raising questions about its practicality in modern healthcare settings.
Patient Perception: Trust and Approachability
Does wearing a white coat actually influence how patients perceive their doctors? A large-scale study conducted by researchers at the University of Michigan, involving 4,000 patients across 10 U.S. academic medical centers, sought to answer this question. The findings, published in BMJ Open, revealed that physician attire does indeed impact patient perceptions and satisfaction with care.
The study demonstrated that patients viewed doctors wearing white coats over business attire (navy blue suit and dress shoes) as significantly more knowledgeable, trustworthy, caring, and approachable. This was particularly pronounced among patients aged 65 and older. Doctors in scrubs with a white coat also scored highly, followed by those in business attire alone. Interestingly, in specific settings like operating rooms and emergency departments, patients expressed a preference for doctors in scrubs only, suggesting context matters in attire preferences.
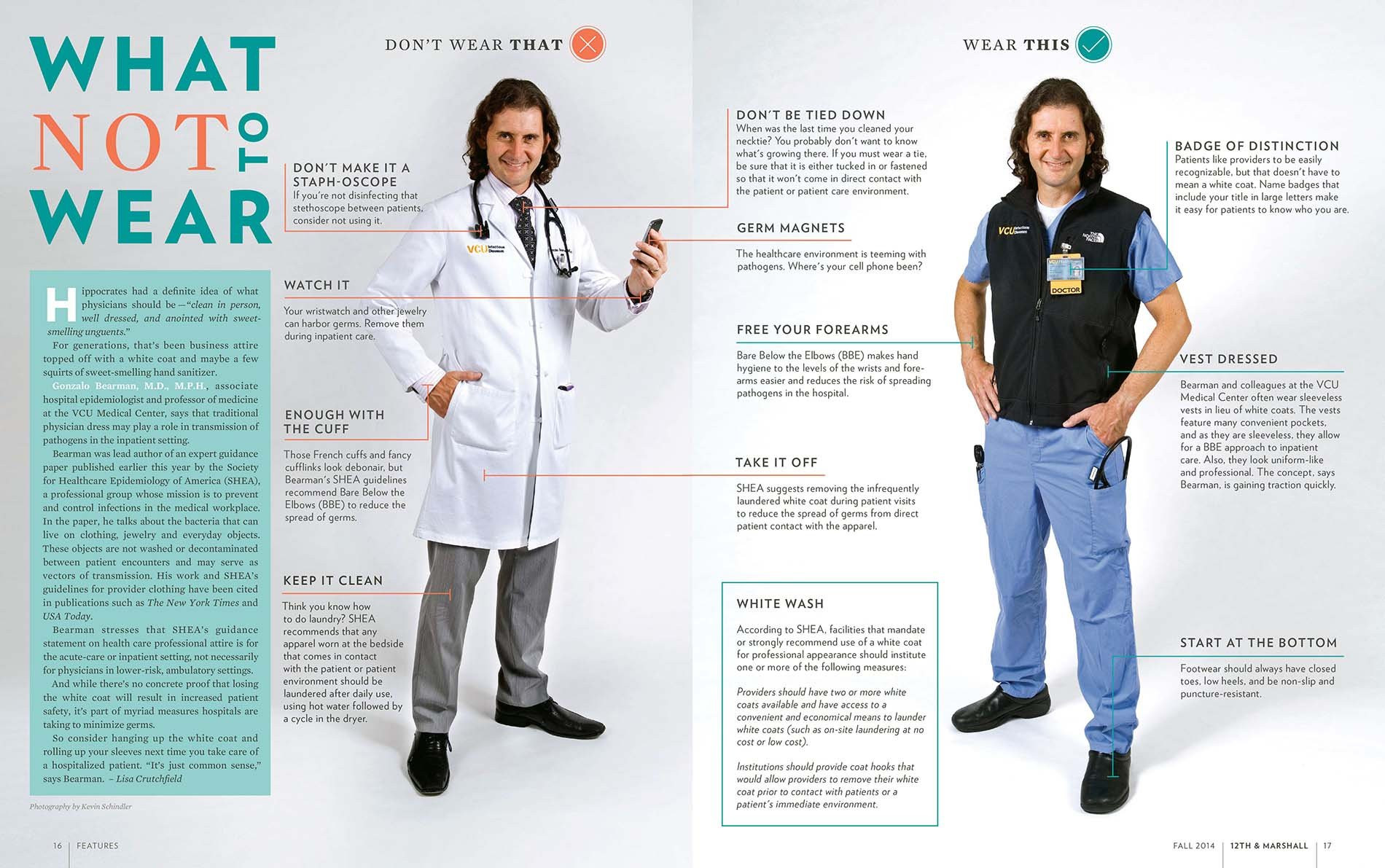 A doctor in two different outfits from Virginia Commonwealth University School of Medicine doctors
A doctor in two different outfits from Virginia Commonwealth University School of Medicine doctors
Two doctors showcasing different professional attire options, highlighting the contrast between business casual and formal wear with a white coat, as presented by Virginia Commonwealth University School of Medicine.
These findings suggest that the white coat, for many patients, continues to serve as a visual cue of competence and authority, fostering trust and confidence in their physician’s abilities. As Dr. Christopher Petrilli, lead author of the study, points out, “At a time when we’re all trying to be more patient-centered, doesn’t it make sense to do what people want?”
However, it’s important to note that not all patient populations and medical specialties favor the white coat. Pediatricians and psychiatrists, for example, have increasingly opted to forgo white coats, recognizing that they can be intimidating or anxiety-inducing for children and patients with mental health conditions. The Mayo Clinic, a renowned medical institution, even instructs its physicians to wear business attire only, aiming to foster a more relaxed and less hierarchical doctor-patient relationship.
The Hygiene Hypothesis: White Coats as Vectors for Germs
While the white coat may project an image of cleanliness, the reality is more complex. Numerous studies have highlighted the potential for white coats to harbor bacteria, including potentially dangerous microbes. Concerns about white coats as vectors for hospital-acquired infections are not new. As early as 1991, a UK study raised awareness about the microbial contamination of white coats, and subsequent research has consistently corroborated these findings.
By 2007, the BBC declared the white coat “more or less dead” in the context of hygiene concerns. In 2008, the UK’s National Health Service, already wary of white coats creating barriers, mandated that physicians wearing them must be “bare below the elbows” to minimize the risk of contamination. The American Medical Association even considered a ban on white coats in hospitals in 2009, reflecting the growing unease within the medical community.
Dr. Mike Edmond, an infectious disease expert, emphasizes the practical concerns, stating, “Asking patients what they want doctors to wear isn’t even a valid question. No patient picks their doctor that way.” He points to the evidence of white coats carrying germs, particularly on cuffs and pockets, areas prone to contact and less frequent cleaning.
Studies reveal that while other patient-contact items are routinely sanitized or disposed of, doctors often launder their white coats infrequently. Reports indicate that physicians may wash their lab coats as little as once every 12 days, and a significant percentage admit to rarely, if ever, laundering their neckties, further compounding hygiene concerns.
Short Sleeves and Sleeveless Vests: Practical Alternatives?
In response to hygiene concerns, some experts propose practical solutions that allow doctors to retain the symbolic white coat while mitigating infection risks. Rolling up sleeves is one simple yet effective measure. A 2017 study led by Dr. Amrita John demonstrated that long sleeves significantly contribute to cross-contamination. Her research showed that healthcare workers wearing long-sleeved coats were more likely to contaminate their coats and transfer pathogens compared to those with short sleeves.
Dr. John advocates for short-sleeved white coats as a balanced approach. “In my medical school training in India, we didn’t want to have a barrier between patients and us. But it’s true many people expect doctors to wear them.” Short sleeves address both patient expectations and hygiene considerations, reducing the surface area for potential contamination.
Virginia Commonwealth University School of Medicine has taken a more innovative approach, providing doctors with sleeveless black neoprene vests. These vests offer the practicality of pockets and warmth without the sleeves that can harbor germs. Dr. Gonzalo Bearman highlights the benefits: “The vest keeps doctors warm but doesn’t restrict movement… And we’ve now got between 70 to 80% compliance with bare-below-the-elbows, without a hard mandate. There’s no evidence this reduces infections, but it’s a common-sense intervention.”
White Coat Syndrome: Anxiety and Blood Pressure
Beyond hygiene, the white coat is also implicated in “white coat syndrome,” a phenomenon recognized since 1896. This syndrome describes the elevation of blood pressure in patients solely due to the anxiety associated with being in a medical environment and interacting with healthcare professionals, often symbolized by the white coat. Studies suggest that white coat syndrome can affect up to 30% of patients.
Emerging research indicates that white coat hypertension is not a benign condition. A mortality study published in the New England Journal of Medicine revealed that patients with white coat hypertension have twice the risk of death compared to individuals with normal blood pressure. This underscores the importance of managing patient anxiety and considering the potential impact of the white coat on patient well-being.
Rethinking Hierarchy: The Length of the Coat
Even the length of the white coat has become a symbol laden with meaning, particularly within medical training hierarchies. Traditionally, first-year residents wore short, hip-length coats, while more experienced residents and attending physicians donned longer, knee-length coats. This visual distinction, while perhaps subtle to patients, was a clear marker of rank within the medical profession.
However, this tradition is also facing scrutiny. The Osler Medical Residency Training Program at Johns Hopkins Hospital, the oldest residency program in the US, recently abandoned the practice of short white coats for first-year residents. New doctors expressed that the short coat symbolized a hierarchical system that placed them below their senior colleagues.
Dr. Sanjay Desai, director of the residency program, acknowledges the historical rationale behind the short coat, stating it was rooted in the idea that “just because you earned your MD doesn’t yet mean you are a clinician.” However, recognizing the negative connotations perceived by contemporary medical students, the program opted for a more egalitarian approach. “Students interpreted the short white coat as a physical symbol of hierarchy and rigidity, so we eliminated it,” explains Dr. Desai.
This shift reflects a broader trend toward flattening hierarchies in medicine, fostering a more collaborative and team-oriented environment. Critics of coat-length hierarchies argue that they can hinder patient safety by discouraging junior doctors from speaking up when they observe potential errors by senior physicians.
The White Coat: An Enduring Symbol in Evolution
Will the white coat disappear from the medical landscape? Probably not entirely. Despite the ongoing debates and evolving perspectives, the white coat remains a powerful and deeply ingrained symbol of the medical profession. As Dr. Paul Sax notes, the topic elicits strong opinions on both sides, highlighting its continued relevance and emotional resonance within medicine.
Ultimately, the future of the doctor’s white coat may lie in adaptation and mindful usage. While some physicians may choose to forgo it altogether, many will likely continue to embrace it, recognizing its symbolic value for patients and their own sense of professional identity. The key, perhaps, is to strike a balance – leveraging the positive aspects of the white coat while addressing legitimate concerns about hygiene, patient anxiety, and hierarchical implications. Whether it’s through short sleeves, sleeveless vests, or more frequent laundering, the white coat is likely to remain a topic of discussion and evolution within the ever-changing world of medicine.
In the words of Dr. Desai, “I don’t wear it every day, but I do when I am in front of patients. It’s part of the process for me. It’s almost a uniform for when we want to help patients feel better.” This sentiment encapsulates the enduring appeal of the white coat – a symbol that, despite its complexities, continues to represent the doctor’s commitment to healing and patient care.
