ProPublica is a nonprofit newsroom that investigates abuses of power. Sign up to receive our biggest stories as soon as they’re published.
Lisa Warwick found her husband struggling to breathe at the bottom of their basement stairs, a harrowing realization that their miracle was ending. It was August 2, 2020, over eleven years since Scot Warwick’s diagnosis of Stage 4 lung cancer. A diagnosis typically measured in months, but Scot, who had just turned 51, had defied all odds.
“Are we going in?” she asked, her voice tight with apprehension.
“Yes,” he gasped. “We are going in.”
His body had weathered six years of relentless chemotherapy and another five of experimental treatments. His medical records noted a “singularly impressive” response. Just two months prior, he was running five miles a day, but the latest chemotherapy round had triggered a rapid decline.
Lisa Warwick helped her husband ascend the stairs, practically dragged him to their car, and sped to St. Peter’s Hospital in downtown Helena, Montana.
The emergency room physician noted shortness of breath, fever, and chills. He highlighted that Warwick’s respiratory distress might stem from the recent chemotherapy, restarted weeks earlier by his diagnosing oncologist, the only doctor he had consistently seen for over a decade: Doctor Weiner.
The following morning, Dr. Randy Sasich began his shift at St. Peter’s. This independent nonprofit hospital, with just under 100 beds, serves as the sole acute-care facility within a 100-mile radius, impacting generations of area residents. Helena, Montana’s capital, retains its Old West charm with a population of only 34,000, making doctor recruitment a persistent challenge. This was particularly true in April 2020, at the pandemic’s onset, when Sasich signed a short-term contract.
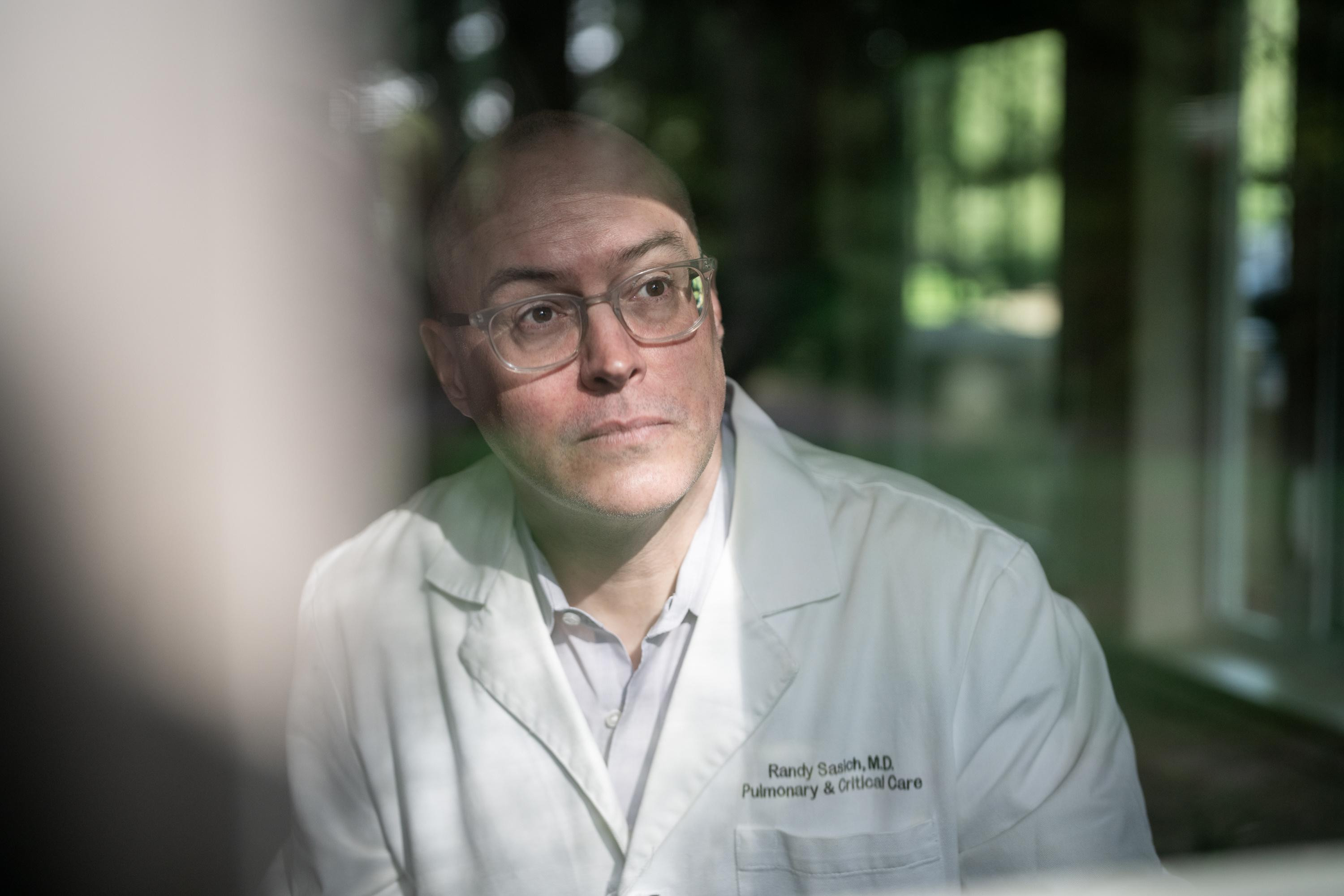 Dr. Randy Sasich
Dr. Randy Sasich
Dr. Randy Sasich, a 47-year-old lung specialist with degrees from Georgetown and Santa Clara University and experience in major city hospitals, was a significant acquisition. As the de facto director of the hospital’s intensive care unit, Sasich met with the morning shift’s coordinating doctor in the ICU, reviewing patients and their needs. Then they reached Warwick’s case.
“We have a 51-year-old patient with metastatic lung cancer, diagnosed 11 years ago,” Sasich recalled the doctor saying.
“There’s no way,” Sasich interjected, disbelief coloring his tone.
“Well, he’s been treated for 11 years,” the doctor clarified.
“You don’t live 11 years after a Stage 4 lung cancer diagnosis,” Sasich stated firmly. “That doesn’t make any sense.”
What We’re Watching
During Donald Trump’s second presidency, ProPublica will focus on the areas most in need of scrutiny. Here are some of the issues our reporters will be watching — and how to get in touch with them securely.
 ProPublica Reporters Trump
ProPublica Reporters Trump
 Photo of Maryam Jameel
Photo of Maryam Jameel
Maryam Jameel
I’m an engagement reporter interested in immigration, labor and the federal workforce.
 Photo of Jesse Coburn
Photo of Jesse Coburn
Jesse Coburn
I’m tracking how the Trump administration reshapes policy at the Department of Housing and Urban Development and the Department of Transportation.
Robert Faturechi
I have been reporting on Trump Media, the parent company of Truth Social. I’m also reporting on the Trump administration’s trade policies, including tariffs.
Sharon Lerner
I cover health and the environment and the agencies that govern them, including the Environmental Protection Agency.
 Federal Govt Callout
Federal Govt Callout
We’re trying something new. Was it helpful?
Between patient consultations, Dr. Sasich meticulously reviewed Warwick’s chart. He thought there must be a misunderstanding, a medical game of telephone gone awry, or perhaps a breakthrough in cancer treatment he was unaware of. He located the 2009 report that initiated the cancer diagnosis. Warwick, a smoker at the time, had consulted an ear, nose, and throat doctor about a minor neck lump. The ENT specialist had sent a sample of cells from Warwick’s neck to the lab. Days later, he noted in the file that the cells were “most likely consistent” with cancer.
That is not a cancer diagnosis, Sasich realized with growing unease.
The records indicated Warwick was referred to the hospital’s Cancer Treatment Center, then under the direction of Dr. Thomas C. Weiner. Sasich’s curiosity escalated to alarm: there was no biopsy. Yet, Warwick was immediately placed on an aggressive chemotherapy regimen by Dr. Weiner, the hospital’s sole oncologist.
This is deeply concerning.
In his short tenure at St. Peter’s, Sasich had already questioned Dr. Weiner’s incomplete documentation and questionable diagnoses, seeking counsel from a senior doctor. To Sasich’s astonishment, his colleague feared challenging Dr. Weiner. According to Sasich, the doctor confessed, “I live here. My kids go to school here. I don’t want to move.”
Sasich meticulously examined Warwick’s file, searching for evidence of a lung tissue biopsy that would capture more cells and pinpoint the disease’s origin. Where was the lab report confirming cancer and ruling out other possibilities? From 2009 to 2019, he found nothing. Then, finally, in April 2020, just months earlier, he found a report on biopsied lung cells. Sasich reread the pathologist’s conclusion: no cancer.
“What the hell is going on here?” he whispered, the implications chilling him.
Despite the negative biopsy, Dr. Weiner had initiated another chemotherapy round for Warwick, according to medical records. Within two months, Warwick had become too weak to climb stairs, and now he was in the ICU, while his wife and children waited outside, COVID-19 protocols keeping them separated.
Sasich contacted the pathologist, who verified the negative finding. Sasich began to fear his own hypothesis. He worried about the impact on Warwick and his family, but the “unbelievable conclusion” forming in his mind might actually save the patient’s life.
The next morning, Sasich entered the dimly lit ICU room where Warwick lay, oxygen being administered. Sasich wrestled with how to tell a man that everything he had believed about himself for over a decade was a fabrication.
Deposition of Dr. Randy Sasich
Moments after Sasich left, Warwick called his wife, agitated. “He doesn’t know my history,” he told her. “He doesn’t know anything about me. He doesn’t know I’ve had this for 11 years. He doesn’t know anything. And this doctor’s telling me that I don’t have cancer? This guy’s an idiot.”
Sasich was aware he had challenged a powerful figure in Helena. He was just beginning to understand the extent of that power, the kingdom built by Doctor Weiner.
While reporting on the COVID-19 crisis in early 2022, I found myself in Helena, in conversation with several St. Peter’s medical staff. They questioned why I wasn’t investigating Tom Weiner. There was a deeper, more disturbing narrative, they hinted, about the oncologist many within the hospital suspected of harming his patients. Despite these hushed concerns, Dr. Weiner was adored by countless patients— “followers,” some staff called them. His nurses were intensely loyal— “a cult,” others whispered. Even hospital administration seemed to fear him.
The rumors, though vague, were unsettling and impossible to dismiss. They depicted a man whose capacity to inspire and intimidate had deeply divided Helena. It would take two years to unravel the myth surrounding Dr. Weiner, the hospital’s role in its creation, and the attempts to conceal a trail of suspicious deaths. One of these, I would later discover, was a 16-year-old girl.
Early in my investigation, I contacted Dr. Weiner. Initially hesitant, he eventually agreed to an interview. He insisted he was the “good guy” in this story.
 Dr. Thomas C. Weiner
Dr. Thomas C. Weiner
Dr. Thomas C. Weiner, 61, is a private individual. Raised Lutheran, his mother was a nurse, and his father, an FBI agent, encouraged him to pursue law. Doctor Weiner told me he was “never much of a research guy.” Instead, he sought to bring a personal touch to medicine, supporting people during their most vulnerable times. He attended medical school at Hahnemann University, now Drexel, in Philadelphia. There, he met his wife, a devout Catholic, and converted. Drawn to the American West’s rugged appeal, a keen mountain climber and skier, Doctor Weiner, after training in Pennsylvania and Vermont hospitals, accepted a position at St. Peter’s in 1996.
He arrived as a beacon of hope. A Great Falls Tribune advertisement announced the hospital’s hiring of a permanent oncologist to lead its new cancer treatment center, replacing a rotation of commuting doctors. For nearly 24 years, he was the only oncologist available to thousands of cancer patients in the region. It’s no exaggeration to say that anyone touched by cancer during that time knew of Doctor Weiner.
He quickly gained popularity. Among his early patients was fashion designer Liz Claiborne, whose husband described Dr. Weiner as “a solid rock of a man, cheerfully youthful, robust, square-shouldered, handsome in a quiet way.” The Weiners became active members of the Cathedral of St. Helena and donated to the Vatican.
In our conversations, he resembled Claiborne’s husband’s description, though weathered by decades in Montana’s harsh climate. Fit, often in hiking shoes, a North Face T-shirt in warm weather, fleece when cold. With piercing blue eyes, he smiled confidently as he explained his medical judgments, radiating absolute conviction in his beliefs and actions as Doctor Weiner.
Doctor Weiner’s reputation grew alongside the cancer center’s. By late 2000, it was treating around 250 patients annually. Three months later, expansion plans included six more chemotherapy chairs, a library, and a meditation center. An Independent Record article noted, “In the five years that Doctor Weiner has been with the cancer treatment center, he has seen an increase from 12 or 13 patients per day to 35 or 40 patients per day.”
Doctor Weiner told me, and records confirm, he billed for up to 70 patient contacts daily. This pace made him an extreme outlier in federal insurance regulator data, yet no one at the hospital intervened. He spoke proudly of his workload, claiming to be constantly on call and providing his cell phone number to many patients. As the cancer center thrived, so did Doctor Weiner’s financial success.
Deposition of Dr. Thomas C. Weiner
Adding to his substantial base salary, his income was calculated by relative value units, or RVUs, billed on behalf of the hospital. This system compensates doctors based on weighted values for visits and treatments. For instance, a doctor might earn $100 per RVU. A routine physical might equal 1 RVU, or $100; a complex procedure like radiation therapy could equal 8 RVUs, or $800. Essentially, more patient visits and treatments billed to insurance meant higher earnings for both Doctor Weiner and the hospital. Doctor Weiner described this common American medical compensation model as “eat what you kill.”
In 2006, Doctor Weiner purchased a 3,400-square-foot home atop Mount Helena with panoramic city views. The following year, his soaring RVUs made him the hospital’s top earner at $751,000, tax filings reveal. By 2010, Doctor Weiner’s income exceeded $1.3 million, more than triple that of hospital CEO John Solheim.
Around this time, hospital administrators worried that Doctor Weiner’s compensation could attract scrutiny from federal regulators for Stark Law violations, prohibiting physicians billing Medicare and Medicaid from self-enriching patient referrals, court records show. These programs constituted about 60% of St. Peter’s revenue. As pay concerns intensified, Doctor Weiner reportedly orchestrated a staff rebellion via text messages. A majority of St. Peter’s medical staff signed a no-confidence letter in Solheim, and Doctor Weiner spearheaded a letter in the Independent Record accusing the hospital of prioritizing profit over patient care quality. Shortly after, Solheim resigned. He did not respond to requests for comment. It’s unclear if the hospital had concurrent concerns about Doctor Weiner’s care quality.
St. Peter’s thrived under Doctor Weiner, recording nearly 200,000 patient visits and over $187 million in revenue in 2012. Doctor Weiner claimed his cancer care accounted for over a quarter of hospital revenue most years; St. Peter’s countered it was closer to 10%.
During pay negotiations, emails show Doctor Weiner leveraged his position as the region’s only oncologist, threatening lawsuits or resignation, consistently prevailing. This power allowed him to control every aspect of his patients’ care by designating himself their primary care physician. With limited local cancer treatment alternatives, patients rarely sought second opinions. Doctor Weiner guarded his domain, resisting attempts to hire another oncologist or transfer patients, court records show. Consequently, few colleagues scrutinized his practice. Insiders termed his setup “his closed system.” As one doctor described, once you were Doctor Weiner’s patient, “he grabbed on to you. He stayed with you for life. No one else would see you until you die.”
Concerns about Doctor Weiner’s billing and patient volume persisted. Solheim’s successor, Nate Olson, also questioned his compensation. Again, Doctor Weiner reportedly helped organize a no-confidence vote, records show. Olson, who also did not respond to requests for comment, resigned in May 2016.
In 2019, St. Peter’s current CEO, Wade Johnson, hired a False Claims Act and fraudulent billing expert to examine Doctor Weiner’s pay. The consultant deemed Doctor Weiner’s RVUs “exceedingly high” and his compensation “a significant outlier.” He logged nearly four times the median oncologist’s visits and treatments nationally, despite serving a sparsely populated area. The consultant warned the billings, while defensible, presented a potential legal and financial liability for both hospital and Doctor Weiner.
From 2009 to 2020, Scot Warwick’s time under his care, the hospital paid Doctor Weiner over $20.1 million. In our discussions, he never avoided income questions. His core argument: without him, St. Peter’s had no cancer center. “You want me to keep seeing everyone?” he’d say. “Then you’re going to pay me more, because I’m doing more work.”
 Helena, Montana
Helena, Montana
Each morning in the ICU, Doctor Weiner visited Warwick, still in gym clothes. Over a decade, Warwick had come to see his doctor as a friend. In their conversations, Doctor Weiner dismissed Sasich’s hypothesis, though he agreed to discontinue gemcitabine chemotherapy. As Sasich spent more time with Warwick, his conviction strengthened. Throughout his treatment, Warwick had shown few lung cancer symptoms, continuing to backpack, camp, and kayak with his children.
Warwick’s records document a medically coded standoff between the local celebrity and the newcomer. Sasich ordered a new biopsy and tests for lung infection. “Dr. Sasich,” Doctor Weiner responded, “is still skeptical of the diagnosis.”
Lisa Warwick first heard from Sasich on August 9, a week into her husband’s hospitalization. He wanted to explain the need for another lung biopsy. A habitual note-taker, she scribbled words her mind resisted: “This doesn’t present to me like cancer,” he told her.
“Well, how could that be?” she recalled thinking. “All our lives sucked for 11 years. I can’t imagine that we went through all that and it not be real.”
Sasich wrestled with his next steps. Doctors rarely challenge each other. But after speaking with the Warwicks, he filed an official complaint, accusing Doctor Weiner of a significant error. He sent a letter to the hospital’s peer review committee, an internal group tasked with examining patient care concerns. He wrote that Warwick “would be the longest living case in the medical literature.”
One test Sasich ordered indicated a possible fungal lung infection—common in immunocompromised patients. Warwick was treated with steroids and antibiotics. He improved and was discharged on August 13 with an oxygen tank. Three days later, Lisa Warwick found him suffocating again. He returned to St. Peter’s by ambulance.
After a week of tests, Sasich told Lisa Warwick her husband was experiencing Stevens-Johnson syndrome, a rare, severe reaction to Bactrim, an antibiotic. It causes skin to blister and peel. Warwick was intubated and airlifted to a specialized burn unit at the University of Utah’s Huntsman hospital. The next day, his left lung collapsed. A doctor urged her to come to Salt Lake City immediately.
For three weeks, Lisa Warwick lived at Huntsman, confined due to COVID-19 restrictions. Doctors there expressed confusion about Warwick’s diagnosis and thin medical history.
When his right lung was near collapse, a doctor asked about his dying wishes—his code status. Do not resuscitate, Lisa Warwick confirmed, a DNR. When they could do no more, the lead doctor pulled her aside. According to court records, he asked if she wanted an autopsy, nodding in encouragement. She agreed.
Scot Warwick’s last communication was a faint hand squeeze. He died just after midnight on Wednesday, September 16, 2020.
 A memorial to Scot Warwick
A memorial to Scot Warwick
About a month later, his widow received a call from the medical examiner. She recalled the conversation during court testimony:
“Mrs. Warwick, I’ve never had to make this call before,” he began. She started taking notes. “I’m sorry.”
“OK?”
“We did not find any cancer cells at all. We can’t find anywhere in his records that he had cancer and found no malignancy at all.” All indications pointed to lung failure caused by gemcitabine. Chemotherapy had killed him, not cancer, and certainly not Doctor Weiner’s purported miracle cures.
As the call ended, she asked, “What am I supposed to do with this? What do I do?”
“Get a lawyer,” he advised.
 The Warwick family
The Warwick family
After Warwick’s death, Sasich encountered Dr. Robert LaClair, the hospital’s kidney specialist and peer review committee chair. “How the fuck did this go on for so long?” Sasich asked. He respected LaClair and often consulted him. LaClair’s expression made Sasich fear he’d offended him.
LaClair, a former Air Force doctor, valued bureaucratic process, unlike Sasich. LaClair had worked with Doctor Weiner for 11 years, suppressing his concerns. As he later told me, “I was caught up in the culture. We all were.”
LaClair revealed he had been quietly building a case against Doctor Weiner for months. According to court testimony, he advised Sasich to stay quiet; removing Doctor Weiner had to be “by the book.” Doctor Weiner had the resources to sue and had threatened to do so repeatedly. It could become a public spectacle. Sasich was relieved action was being taken but outraged at the delay that cost his patient so much.
LaClair didn’t disclose the full extent. The review had begun a year prior, after LaClair and a colleague questioned Doctor Weiner’s minimal, often illegible, patient notes. This poor documentation hampered follow-up care and, LaClair believed, intentionally obscured Doctor Weiner’s treatment methods. Court records show LaClair and his colleague also instructed Doctor Weiner to stop admitting numerous patients for non-cancer-related stays—financially beneficial to him.
By early 2020, enough confidential complaints from doctors and nurses prompted peer review action. LaClair sent about six patient files to University of Utah medical experts, but COVID-19 delayed conclusions.
After Warwick’s death, St. Peter’s added his file. The reviewing doctor quickly responded, assuming a clerical error: the packet lacked a biopsy supporting the 2009 diagnosis by Doctor Weiner. On October 9, St. Peter’s received his analysis: “If he had cancer, this course of many years would be truly remarkable.” It continued, “The long-term treatment with toxic medications in the absence of a confirmed diagnosis of cancer is not reasonable.”
External reviews are typically cautiously worded. Medicine is complex, with diverse decisions, so doctor reviews often sound deferential. The eight Utah reviews differed.
Examining a 2018 case of a 62-year-old diagnosed with throat cancer by Doctor Weiner, a reviewer described several decisions as potential “malpractice” leading to unnecessary two-month hospitalization. Like Warwick, no biopsy was in the file.
Another review criticized Doctor Weiner’s omissions. A 67-year-old breast cancer patient had chemotherapy, mastectomy, and reconstruction. In a June 2019 check-up, Doctor Weiner noted “no evidence of any recurrence.” But records showed no breast exam. (This was a common failing in his breast cancer treatment.) Months later, the patient found a lump. A biopsy at another hospital confirmed cancer recurrence, requiring a second tissue removal, radiation, and chemo.
Deposition of Dr. Robert LaClair
“I’ve never seen so many cases of what we sent out that was not meeting standard of care. I’ve never seen that before, and I hope I never see it again,” LaClair testified, highlighting the deep concerns surrounding Doctor Weiner’s practices.
LaClair later told me, “When the Utah reports came back, it was like: ‘Holy fucking shit. This is going to suck.’”
On October 15, 2020, St. Peter’s suspended Doctor Weiner and revoked his privileges. Exiled from his kingdom, Doctor Weiner told me he felt “blank.”
The hospital hired The Greeley Company, a healthcare consultancy, to review more patient records, many deceased. Doctor Weiner would have a “fair hearing” to defend himself and regain his position.
News of Doctor Weiner’s suspension devastated his cancer center nurses, his self-proclaimed “Tom’s wives” or “girls.” They were envied for working for Doctor Weiner and the perks. From 2005 to 2020, records show he gave them at least $140,000 in bonuses and jewelry. Retirement gifts included diamond solitaire earrings worth about $1,500. He hosted dinners and holiday parties. They regularly messaged him well wishes during his Italy trips.
Following his suspension, they delivered food and supportive notes, vowing resistance. Doctor Weiner urged them not to jeopardize their jobs for him.
“I love you. I’m here. I’m so sorry. I’m praying,” nurse Emily Burton texted him.
“You can tell the girls I will be fighting,” Doctor Weiner responded. “But it will probably get bloody.”
To others, like nurse Meghan Giovenco, he expressed anger: “They are going for the jugular. Scum.”
When Doctor Weiner learned Sasich questioned his work before his nurses, he texted a hospital administrator, “FYI put a muzzle on Sasich or else.”
News of Doctor Weiner’s suspension spread through Helena. Patients formed a Facebook group, “We stand with Dr. Tom Weiner.” He saved lives, they said. He remembered their families. He was kind, brilliant. Hundreds joined.
Inside St. Peter’s, it resembled the campaigns that ousted prior CEOs—worse. Rallies began outside the hospital. Ousting the region’s only oncologist, they argued, abandoned patients to long waits and rotating travel doctors. One sign read, “I WANT MY DR. WEINER, NOT THE SECOND STRING.” Yard signs, bumper stickers, and T-shirts appeared. Supporters caravanned downtown, honking.
 Signs of support for Dr. Weiner in Helena
Signs of support for Dr. Weiner in Helena
 Signs of support for Dr. Weiner in Helena
Signs of support for Dr. Weiner in Helena
Public displays of support for Dr. Weiner emerged in Helena, reflecting the community’s deep division over his suspension.
The hospital fired Doctor Weiner on November 17, 2020. CEO Johnson convened a cancer staff meeting, calling Warwick’s death “the tip of the iceberg.” He forbade recordings, court documents show, and the chief nurse instructed employees to put away phones. All of Doctor Weiner’s patients should seek second opinions, Johnson advised.
Johnson also warned staff, “Don’t be surprised if black suits show up.” Doctor Weiner’s nurses understood this to mean federal law enforcement or HHS investigations. “He explained it to be suits—there were going to be suits coming into the office and asking for things,” nurse Andrea Thies testified, taking notes despite the order.
“You walked out of there feeling like, ‘Was I killing people?’” nurse Fallon Melby later testified, reflecting the profound impact of the revelations about Doctor Weiner.
Deposition of nurse Fallon Melby
Three weeks later, St. Peter’s posted a shocking disclosure online: “The issues we have identified include the following: harm that was caused to patients by receiving treatments, including chemotherapy, that were not clinically indicated or necessary; failure to meet state and federal laws associated with the prescribing of narcotics; failure to refer patients to other specialists for appropriate treatments; and failure to meet requirements associated with clinical documentation.”
It’s unclear if the hospital reported these issues to the state medical board or law enforcement.
Days later, Doctor Weiner sued St. Peter’s and its executives for wrongful termination and defamation.
In early 2021, Shelly Harkins, the hospital’s chief medical officer, pulled Sasich aside. According to Sasich’s testimony, she apologized for involving him.
Then, she confided a story that made him “physically ill.” Hospital administrators had long suspected a case: a 16-year-old girl who died suddenly under Doctor Weiner’s care. Sasich recalled Harkins’ limited details, but Doctor Weiner was reportedly frustrated by another physician treating his patient. Once Doctor Weiner regained control, the girl died soon after. “She told me that he gave her two doses of propofol,” Sasich testified, “and she died.”
Sasich hoped it was rumor. But when he asked LaClair, the person most knowledgeable about Doctor Weiner’s practice, LaClair didn’t deny it, just corrected one detail. Not propofol.
“No,” LaClair told Sasich. “He uses phenobarbital.”
 St. Peter’s Health CEO Wade Johnson
St. Peter’s Health CEO Wade Johnson
Post-Weiner’s termination, dozens of his patients sought opioid refills. Doctors taking over his caseload couldn’t find prescriptions in St. Peter’s system, court records show, and Doctor Weiner’s files were unhelpful. They turned to a state database tracking pharmacy opioid sales, discovering he had been writing prescriptions by hand, bypassing hospital controls. Shockingly, many patients were on dangerously high narcotic levels for years. The state agency overseeing the registry didn’t respond to requests for comment.
Often, patients seeking painkillers had no cancer or documented need. Doctor Weiner had prescribed them as their primary care physician. Many struggled with addiction. St. Peter’s created a document to track the crisis, noting “nonsensical” prescriptions and “one of the worst indications for opioids. I’m still piecing this together …” and “Many years on methadone. Not clear why.”
Doctor Weiner claimed the hospital fabricated these allegations to justify his firing, denying handwritten prescriptions.
St. Peter’s assembled pain management experts to review over 2,000 patient files. Dr. Kyle Moore, an addiction specialist, led detox efforts. He found Doctor Weiner rarely accounted for morphine equivalents, risking lethal doses. Doctor Weiner denied this. In a narcotics tracking memo, Moore is quoted calling Doctor Weiner’s prescribing “a greater danger to the community than coronavirus.”
Narcotics Tracking Memo– Observations from Dr. Moore
Stated Dr. Weiner’s prescribing practices “are a greater danger to the community than coronavirus.”
Failure to follow appropriate protocols for safe prescribing
Practicing beyond scope (seeing many pain patients who do not have active cancer or cancer-related pain being treated w/ high dose opioids)
Meds and dosage prescribed non-sensical
The full scope of Doctor Weiner’s prescription practices may remain unknown. The hospital alerted the DEA, which began an investigation, a spokesperson confirmed. But court records show no St. Peter’s attempt to quantify the problem beyond initial detox efforts. St. Peter’s wouldn’t say if it sought overdosed or deceased patients in the community or reported findings to the state medical board.
While doctors taking over patients were horrified, court records reveal hospital administrators and the peer review committee were warned over a dozen times since at least 2018 about Doctor Weiner’s overprescribing. Staff who raised concerns feared Doctor Weiner’s intimidation. In 2019, two nurses and a pharmacist questioned Doctor Weiner’s fentanyl patch order for a 93-year-old already on opioids and fading in and out of consciousness. A nurse texted Doctor Weiner for confirmation. Doctor Weiner responded, “Tell them put it on or I will rip their lips off.” Doctor Weiner called this “an inside joke.”
Federal regulators also missed alarming trends. Medicare data shows, from 2013 to 2020, Doctor Weiner’s opioid prescription volume ranked ninth among all cancer doctors billing the program. For morphine, he consistently ranked top five, even number one in 2017. CMS didn’t respond to questions.
Before firing Doctor Weiner, St. Peter’s sent five pain management cases to The Greeley Company. All were inappropriate. One was Sharon Dibble, 75, with multiple health issues, including kidney failure and COPD.
On March 6, 2018, inexplicably to reviewers, Doctor Weiner doubled her extended-release morphine from 30 to 60 milligrams twice daily, atop oxycodone. Four days later, Dibble’s daughter found her unresponsive, blue, not breathing. Paramedics rushed Dibble to St. Peter’s, where she was on life support for over two weeks. She died March 27.
St. Peter’s cited acute respiratory failure. The family believed her ailments overwhelmed her. But the Greeley review concluded Doctor Weiner’s “excessively large increase” in morphine “led to respiratory arrest and the patient’s demise.”
The Greeley Findings on Sharon Dibble’s Death
This can be a challenging situation to manage, and there was at least some documentation of appropriate shared decision making with the patient regarding the risk of addiction to opioids. However, this does not justify the excessively large increase in the MS Contin dose that led to respiratory arrest and the patient’s demise.
When I discussed the Greeley review with Doctor Weiner, he called it “ridiculous.” He claimed he swapped short-acting for long-acting pain medicine, keeping Dibble’s morphine equivalent unchanged—contradicted by records and the hospital review. The CDC cautions against exceeding 90 morphine milligrams daily, warning over 120 risks overdose. Records show Dibble’s regimen equaled 195 milligrams.
St. Peter’s never informed Dibble’s family of its findings regarding Doctor Weiner’s role.
Five years after Dibble’s death, I shared the report with her children. Tom Dibble, her son, had decided to stop life support, believing it was her time. Now, he feels deceived.
“Not only did this individual cause her death,” he said of Doctor Weiner, “but it’s pretty apparent that this whole thing was being covered up. We were never given any knowledge that this took place, and we have to live with this decision.”
 Family of Sharon Dibble
Family of Sharon Dibble
Family photographs of Sharon Dibble, and her children Cindy White, Tom Stevison, and Melba VanSprang, along with her husband, Dennis Dibble, who are now grappling with the findings about Dr. Weiner’s role in her death.
Six months after Doctor Weiner’s firing, the hospital held its fair hearing. Like a trial, with witness testimony and cross-examination, but private, judged by three St. Peter’s doctors. On night one, LaClair detailed the allegations—Warwick’s death, misdiagnoses, narcotics, and more, all linked to the questionable practices of Doctor Weiner.
But the worst accusation was Doctor Weiner overriding patients’ dying wishes. Patients wanting CPR or breathing machines are “full code.” Doctor Weiner, the hospital argued, routinely changed patients’ status to DNR/DNI without consent. The hospital wouldn’t confirm if it fully investigated what the panel deemed “a serious violation of the standard of care and medical ethics” by Doctor Weiner.
At the hearing, nurse Addie Weidow described two instances of code status changes without permission, one patient nearly dying before another doctor intervened. In another case, a full-code patient’s chart suddenly read DNR/DNI. Nurses tried to apply a DNR wristband; when the patient refused, Weidow testified Doctor Weiner instructed them to “hang the band on the doorknob and leave it be”—a “slow code,” Weidow testified, orchestrated by Doctor Weiner.
After Doctor Weiner left, Dr. Ashley Coggins managed his patients, gaining insight into his closed system. She testified “many nurses have come to me in the last several years, telling me that that was a standard practice of his—to just change people’s code statuses once they were doing poorly.” She added: “He was basically using his own judgment as the judgment for people to live or die. It’s horrifying,” highlighting the ethical breaches allegedly committed by Doctor Weiner.
During the hearing, a hospital attorney questioned Dr. Kerry Hale about the 16-year-old girl, the rumor haunting Sasich. Hale recalled a girl with Wilms tumor, a childhood kidney cancer, treated on pediatrics, then transferred to Doctor Weiner’s oncology floor “and then orders for DNR, and then three doses of phenobarbital were given, and the patient died, I believe, that evening.” Phenobarbital, a barbiturate for seizures during alcohol withdrawal, is lethal in large doses, and allegedly used by Doctor Weiner.
When Doctor Weiner’s turn came, his lawyer asked for his account. His answer was clinical. “Mom wanted her comfortable,” he said. “So, I transferred her to the oncology floor, and I gave her pain meds, phenobarbital, and she died later,” a chillingly detached explanation of his actions regarding the young patient. Neither hospital nor Doctor Weiner’s attorneys pressed for details.
“Comfort” was Doctor Weiner’s common term. If treatment causes death, it’s ethical if the intent is comfort, he told me, invoking the principle of double effect, from Thomas Aquinas. Harmful consequences, like death, are permissible if secondary to beneficial treatment, like pain relief. “It’s for their comfort,” Doctor Weiner told me. “It’s not that I euthanize them,” an attempt to rationalize his controversial end-of-life care practices.
At the fair hearing, Doctor Weiner denied all hospital accusations. “Part of my problem is I have a good memory,” he said, “so I just remember things, and I probably should put more in the chart.” High-dose opioids weren’t unusual; he’s an oncologist, patients suffer. Painkillers for non-cancer patients? St. Peter’s lacked a pain specialist for most of his tenure, he claimed, deflecting criticism of his practices.
Regarding end-of-life care, Doctor Weiner claimed he discussed options with “tens of thousands” of patients before changing their code status, a broad, unverified assertion.
The panel unanimously rejected Doctor Weiner’s appeal.
 St. Peter’s Hospital
St. Peter’s Hospital
Despite firing, Doctor Weiner kept his medical license. The hospital only reported his suspension, not its findings, to the state medical board and National Practitioner Data Bank. The medical board wouldn’t comment on a Doctor Weiner investigation.
Instead of retiring or private practice, Doctor Weiner sued St. Peter’s, spending millions, expecting a $20 million settlement because “they can’t let out what they did,” confident in his ability to leverage secrets.
By suing, Doctor Weiner exposed himself and St. Peter’s to discovery. Over three years, thousands of documents—texts, patient files, financials, hearing transcripts—became court evidence, detailing the extent of Doctor Weiner’s alleged misconduct. Doctors, nurses, administrators, and Doctor Weiner himself gave depositions.
Though adversaries, Doctor Weiner and St. Peter’s shared a goal: concealing evidence. They successfully sealed most discovery. I obtained it, revealing the inner workings of Doctor Weiner’s kingdom.
Had Helena residents seen these files, they’d understand how Doctor Weiner built a high-volume practice billing public and private insurance extensively, subjecting patients to unnecessary, life-threatening treatments. They’d see the hospital’s financial incentive to ignore it, and the true cost of Doctor Weiner’s reign.
High-volume business evidence was public in CMS data. Medicare Part B data from 2013-2020 showed Doctor Weiner billed 40,000 15-minute visits, more than any US doctor of any specialty. Public data hinted at a larger problem St. Peter’s knew: “He’d see 15 patients in 30 minutes,” LaClair told me, illustrating the unsustainable pace driven by Doctor Weiner. This enriched Doctor Weiner and seemingly escaped insurance regulator attention.
Why did CMS miss Doctor Weiner’s outlier status? John Hargraves, a Health Care Cost Institute data expert, explained CMS looks for blatant fraud, like billing for pricier services than provided. Doctor Weiner instead crammed in an extreme number of low-cost visits, a loophole in oversight.
When asked, St. Peter’s didn’t refute findings but broadly declined comment, citing litigation. “We believe this situation is isolated to a single, former physician, and we remain confident in the exceptional care provided by St. Peter’s medical staff,” spokesperson Andrea Groom emailed, downplaying systemic issues and focusing blame solely on Doctor Weiner.
In a follow-up, Groom wrote, “Dr. Weiner was a highly productive physician, but this was not necessarily alarming, given that he was the only medical oncologist treating cancer patients for a large service area during much of his time with St. Peter’s Health.” Patient satisfaction was high, complaints rare, and “there was no reason at the time for St. Peter’s to believe that Dr. Weiner was providing substandard care,” a statement that now rings hollow in light of the evidence.
In court filings, St. Peter’s admitted expecting more lawsuits from Doctor Weiner’s patients, acknowledging the potential scale of harm.
The hospital response ignores St. Peter’s enabling and protecting Doctor Weiner. As LaClair said, colleagues didn’t intervene earlier “because we were afraid of him,” highlighting the culture of fear surrounding Doctor Weiner. St. Peter’s admitted in filings knowing for years of “serious concerns of physician colleagues and staff members with several patient deaths” linked to Doctor Weiner. When asked why the hospital publicly accused him of malpractice but withheld end-of-life care concerns, Doctor Weiner claimed administrators knew and encouraged it, implying deeper complicity.
Fifteen months before firing, Doctor Weiner and his nurses took over hospital end-of-life care. An August 2019 text exchange between chief nurse Kari Koehler and Doctor Weiner formalized it: “Are you still okay if all end of life patients go to onc[ology] even if they aren’t yours? I just feel like those nurses do it best!”
Doctor Weiner replied: “I agree!!” solidifying his control over end-of-life protocols.
By summer 2021, the pro-Weiner Facebook group had ~4,000 members. The hospital CEO was “evil,” “a true devil,” “puke.” They successfully campaigned to name Doctor Weiner “Helena’s Best Physician” in the Independent Record and rented billboards reading “WE STAND WITH DR. WEINER,” showcasing the community’s unwavering support despite the allegations. When asked why Helena was split over him, Doctor Weiner corrected, “I wouldn’t call it 50/50. More like 80/20,” underestimating the depth of division.
For Lisa Warwick and her children, each Weiner sign was a silencing reminder. “I was worried about violence against us,” she said. That summer, they sued St. Peter’s for wrongful death. In her deposition, the widow stated: “My children lost their father. I lost my husband. It wasn’t quick. It was long. And it was torturous. And it was terrible. And I would never, ever wish that on anyone—ever,” encapsulating the devastating personal cost of the alleged medical malpractice.
In depositions and to me, Doctor Weiner insisted Scot Warwick had Stage 4 lung cancer for 11 years. The negative April 2020 biopsy? The pathologist missed the cancer, he claimed. In our talks, Doctor Weiner said cancer moved between Warwick’s lungs.
“He was pretty advanced, though?” I asked. “Don’t you think it would be hard to miss?”
“Well, you would think,” he conceded. “I agree with you. I was kind of pissed off,” a dismissive reaction to serious questions about misdiagnosis.
What about the Utah autopsy doctor? He also missed the cancer, Doctor Weiner said, deflecting all professional scrutiny.
The Warwicks and St. Peter’s settled for an undisclosed sum. Doctor Weiner wasn’t liable as a hospital employee. Why insurers paid for 11 years of Stage 4 cancer treatment remains unclear; none responded to inquiries.
When I mentioned Doctor Weiner’s 80% Helena support claim to Sasich, he didn’t disagree. He drove past protesters to work. In the hospital, Doctor Weiner’s nurses ignored him. The billboards chilled him. He couldn’t fathom why people didn’t demand answers.
 Weiner’s supporters outside St. Peter’s
Weiner’s supporters outside St. Peter’s
The 16-year-old girl’s case haunted him. He replayed Harkins’ and LaClair’s accounts. He asked a hospital lawyer about investigation; “we’re aware,” he was told. He informed Helena’s police chief, and a HHS fraud investigator. No one seemed to pursue it, Sasich said, frustrated by the lack of official interest in potential serious misconduct by Doctor Weiner.
Sasich’s inquiries reached Doctor Weiner, who added him to the defamation suit. Sasich denied it, now entangled in the legal fallout.
Hidden in thousands of hospital documents against Doctor Weiner is a sheet summarizing seven dying patients: “Phenobarbital cases.” Ages 53-77, a small sample of deaths under Doctor Weiner’s care.
The memo tracks a 62-year-old woman admitted for stomach pain October 3, 2018. October 7, 6:01 p.m., she received 260mg phenobarbital for “terminal agitation.” Two hours later, another 260mg, then another at 10:58 p.m.—780mg total. She died just after midnight, one of the phenobarbital cases linked to Doctor Weiner.
The Phenobarbital Memo 1 2 3 4 5 6 7
Total Dosage Summarized from Memo
1 Time of Death: 12/21/19 after 260mg
2 Time of Death: 12/24/19 after 260mg
3 Time of Death: 11/05/19 after 260mg
4 Time of Death: 8/24/19 after 260mg
5 Time of Death: 10/8/18 after 780mg
6 Time of Death: 8/22/18 after 520mg
7 Time of Death: 3/26/18 after 260mg
Unlike narcotics and misdiagnosis cases, these weren’t externally reviewed, but by chief pharmacist Starla Blank. At the fair hearing, Blank found the events alarming as patient proximity to death was unclear. “In most of the cases the patients were talking and visited with Dr. Weiner prior to their—prior to them getting the phenobarbital,” she said, questioning the justification for such heavy sedation in cases overseen by Doctor Weiner.
Yet, St. Peter’s, declining phenobarbital case comment, dismissed Blank’s assessment. Its final account concluded the seven patients “were at end of life and that there were no remaining viable treatment options for them,” a conclusion not universally shared by medical professionals.
One case is missing from the phenobarbital memo: the 16-year-old girl, Nadine Long, whose story is a chilling chapter in the Doctor Weiner saga. Harkins recalled her case but not her name. LaClair offered few details of an unnamed girl. The chief nursing officer mentioned “a child” receiving concerning phenobarbital doses under Doctor Weiner’s care.
An online search for “Thomas Weiner” reveals obituaries thanking the oncologist and nurses. One features Nadine Long, a smiling blonde girl. Her obituary mentions hot air balloon rides, beach trips, a play cabin, lemonade stands, camping, kayaking. Diagnosed with Wilms tumor at 6, she didn’t let it define her, even in the face of Doctor Weiner’s treatment decisions. Her mother quoted her: “Having cancer is no fun, but that doesn’t mean that you can’t have fun just because you have cancer,” a poignant testament to her spirit.
Deposition of Dr. Shelly Harkins
Reasonably sure this was the girl haunting St. Peter’s, I visited Dr. Robert LaClair, the man who finally acted against Doctor Weiner, albeit belatedly.
To my surprise, Dr. LaClair welcomed me. Earlier that week, a Montana judge sided with St. Peter’s, dismissing Doctor Weiner’s lawsuit. The hospital could enforce quality care, the judge ruled, finding no hospital defamation of Doctor Weiner. Doctor Weiner vowed to appeal; his defamation suit against Sasich continues. In LaClair’s study, we discussed Warwick, narcotics, code status—cases he wouldn’t have to recount in court. A weight seemed lifted until Nadine’s name. “Nadine.” His eyes welled. LaClair had read her file but not sent it for review. He exhaled, then, “Trust me, it’s so bad. You have no idea. She wasn’t terminal,” a stark and heartbreaking assessment of Doctor Weiner’s actions.
By June 2024, Doctor Weiner and I had spoken for months. He’d share patient anecdotes, unaware I could identify them and compare his accounts with records. He always portrayed himself as gifted, dedicated. One story was about a dying girl needing his intervention when a less capable doctor failed to provide comfort, setting the stage for confronting him about Nadine Long.
We sat at a long table in a Helena hotel conference room. In jeans and polo shirt, he agreed to recording, mic attached, first discussing a recent Rome trip. Later, I presented a privacy waiver from Nadine’s family, and he recounted her final days, offering his perspective on the Nadine Long case and his broader practices as Doctor Weiner.
It was March 2015. In New York, awaiting “Les Misérables,” Nadine’s mother called, frantic: daughter “in horrible pain. They won’t take care of her pain. Please come home.” Post-show, he flew to Helena, arriving near midnight, driving to St. Peter’s. Nadine was “screaming and crying.”
Doctor Weiner had treated Nadine since childhood, through initial and recurrent cancer. Now, third recurrence. Pleural effusion—lung fluid—restricted breathing. Her mother spoke with Doctor Weiner’s backup, trying to transfer Nadine to St. Jude. Doctor Weiner reviewed scans. “She was going down like a stone,” he told me. “She had hours to a day or two to live. There were no more cards to play,” a dire prognosis offered by Doctor Weiner.
Hearing this, her mother cancelled transfer plans. “She just wanted her comfortable,” Doctor Weiner said. He offered Nadine a choice: aggressive, undignified treatment with no survival promise, or “leave it up to God, and we’re just going to keep her comfortable,” framing end-of-life decisions in spiritual terms, a common tactic of Doctor Weiner.
He moved Nadine to oncology, to his nurses, “and she got some pain meds—I don’t remember how much phenobarbital—and she died later,” a vague account of Nadine’s final hours under his care.
His response mirrored fair hearing testimony. I had reviewed Nadine’s medical record, some of which I presented.
Doctor Weiner examined Nadine less than a week prior. In her file, he wrote, “she looks good…everything looks stable right now.” I asked how he missed the advanced, terminal disease he claimed.
“That’s how fast—the nature of that tumor when it comes back, it comes back with a vengeance,” Doctor Weiner claimed. “That fast,” attempting to justify the rapid shift in Nadine’s condition.
With family consent, I shared Nadine’s records with Dr. Sarah Friebert, Akron Children’s Hospital pediatric oncologist and palliative care center founder. She clarified she spoke for herself, not her employer.
I read Weiner some of her review.
“Here’s a girl who was skiing and then she’s dead a week later, and that’s—that’s concerning,” Friebert told me. “She ate 75% of her dinner on the night she died. Her vitals were not out of whack.” Nadine should have been transferred for testing; nothing definitively showed she was untreatable. Her imminent death wasn’t clear, Friebert stated, contradicting Doctor Weiner’s assessment.
Doctor Weiner’s terminal diagnosis was based on lung fluid tests, insufficient evidence, she said. Neither Friebert nor I found biopsy evidence confirming terminal cancer in Nadine’s file, raising serious questions about the basis of Doctor Weiner’s end-of-life decisions.
Friebert uses phenobarbital for dying children’s comfort, but Doctor Weiner’s escalation “was way out of proportion with what I would ever have done.” Intent couldn’t be comfort. “These doses were obscene,” she said. “He killed her with it,” a damning professional opinion on Doctor Weiner’s treatment of Nadine Long.
That a respected oncologist questioned his care didn’t faze Doctor Weiner. She wasn’t there, couldn’t judge. “I completely disagree,” he said. “This is a girl that’s got—her body is riddled with cancer, and she’s in horrible pain. Now did the phenobarbital hasten her death? Yeah, it did,” a striking admission.
In all conversations, Doctor Weiner insisted his intent was comfort, never hastening death, but here he wavered.
“Could it have shortened her life?” Doctor Weiner asked. “Yes. Again, in most of these cases, could I not give phenobarbital, and would that patient live longer? The answer is yes.” He paused. “But longer in, like, hours? I mean, is that worth being in misery for those hours?” minimizing the potential life shortening and focusing on perceived patient comfort.
“My goal was not to kill Nadine,” he added. “My goal was to make her comfortable,” reiterating his defense.
I’d shown him the “phenobarbital cases” memo, discussed code status changes, Warwick, narcotics, Nadine. Finally, “Are you killing your patients, Doctor Weiner?” I asked directly.
“Well, uh, no. I’m not,” he responded, hesitation evident.
“Why did you hesitate?”
“Well,” he said. “It depends on what you mean by killing them,” a chillingly ambiguous answer from Doctor Weiner.
 Photos of Nadine Long and her parents
Photos of Nadine Long and her parents
Nadine’s parents live outside Helena, at the end of a cattle road around the peak where she played and her ashes rest. Dan Beadle, her father, is a sheriff’s office evidence technician. Cheri Long, her mother, recently retired from Carroll College. They led me to the kitchen table to recount their worst days.
On a 2005 New Hampshire vacation, Nadine was diagnosed with Wilms tumor. Left kidney removed, radiation followed. Back in Montana, they met Doctor Weiner, who oversaw chemo. Nadine bonded with his nurses, “the true loves of her life,” Long said. Remission seemed achieved. But a year later, cancer recurred where her kidney was removed, Doctor Weiner told them. More chemo and treatments until ~2010, when Doctor Weiner declared her cancer-free. Annual check-ups with Doctor Weiner and his nurses continued.
“Dr. Weiner always had a policy that once you’re his patient, he’s your primary physician,” Long said. “I don’t know if that’s normal,” highlighting Doctor Weiner’s unusual control over patient care.
Nadine attended the same Catholic school as Doctor Weiner’s children. Her uniforms were his daughter’s hand-me-downs. Families were friendly, not close. Nadine’s parents respected Doctor Weiner, though Long noted his domineering nature.
Nadine had bipolar disorder. At 14, a psychiatrist noted information processing challenges, “insecurities, anxiety, and tendencies toward frustration when challenged dramatically interfered with her critical thinking skills.” But she was also “kind, compassionate, very empathic,” a complex young woman under Doctor Weiner’s care.
February 2015, Nadine’s parents noticed hunched posture, breathing difficulty. March 2, she saw Doctor Weiner. Brief visit. “He listened to her lungs and said, ‘Everything’s good,’” her father recalled. “Then he tried to palpate a little bit, and she was extremely ticklish, so she started squirming around, and then at some point he goes, ‘I think we’re good to go,’” a seemingly cursory examination just days before her critical condition.
Six days later, skiing, Nadine buckled, fell, rushed to St. Peter’s ER. “Mommy, I’m in the hospital. My lung collapsed,” she called. Parents raced to St. Peter’s. Chest tube inserted, lung fluid drained, but no information. Doctor Weiner was in New York City. For five days in pediatrics, Nadine fluctuated between calm and agitation, vitals stable, while Doctor Weiner remained absent.
They felt misled by Doctor Weiner’s backup. Long requested St. Jude transfer. As arrangements progressed, Doctor Weiner appeared. “Finally,” Long thought, “Someone who’s going to tell us the truth instead of tiptoeing around us,” hopeful for clarity from Doctor Weiner.
Later, she learned a St. Peter’s employee called Doctor Weiner to return. His claim he returned because Long asked for comfort care?
“That’s a flat-out lie,” she told me. “We did not ask for him to come home from his vacation,” directly refuting Doctor Weiner’s narrative.
Doctor Weiner told her a large malignant mass was compressing Nadine’s lungs, soon to suffocate her. “How he described it was, ‘It’s doubling every day, and today it’s the size of a soccer ball,’” Long said, painting a dramatic, rapidly deteriorating picture.
Soon after, Doctor Weiner spoke to Nadine, not her parents. “He told her, ‘You can choose the medical path or the God path,’” Long said. Conversation “between the two of them. We were there, and he would check—he would look at us,” Long recalled. “Taking the God way was saying, ‘I fought my fight, and I’m ready to meet Jesus,’” framing end-of-life as a spiritual choice, influencing a vulnerable teenager under duress.
The information-processing-challenged teenager chose the God path. Parents, fearing suffering, didn’t object. March 13, Nadine changed to DNR/DNI, despite a progress report: “She is alert and oriented, in no acute distress.” Doctor Weiner moved her to oncology, initiating end-of-life protocols.
Nadine was heavily drugged since arrival: Dilaudid, morphine, oxycodone, fentanyl, part of Doctor Weiner’s comfort care regimen. Next day, heart and respiratory rates spiked. Panic. “Saturday afternoon, she’s thrashing, she’s fighting, she can’t breathe,” Long said. Parents and a nurse couldn’t restrain her, witnessing Nadine’s distress under Doctor Weiner’s care. Parents agreed to Doctor Weiner’s “comfort measures.”
Nadine’s file shows phenobarbital ordered.
3:45 p.m.—260mg.
Still thrashing. Nurse nervous about increasing phenobarbital, called Doctor Weiner who oversaw, “He just kept saying, ‘more, more,’” Long recalled, directing escalating sedation.
5:26 p.m.—390mg.
Sedation onset unclear. Doctor Weiner left.
7:47 p.m.—390mg.
Two of Doctor Weiner’s nurses, close to Nadine, stayed late, providing a human element amidst the controversial treatment by Doctor Weiner.
9:54 p.m.—390mg.
Parents relieved pain subsided, held her.
1:45 a.m.—DISCHARGE.
Heart stopped.
Nadine received 1,430mg phenobarbital. Adult dose: 260mg. She weighed 100 pounds, a massive overdose under Doctor Weiner’s orders.
Dr. Thomas Weiner’s Note Following Nadine Long’s Death– ADMITTED 03/08/2015
- DISCHARGED 03/14/2015
I had a long discussion with the family and the patient and she really did not want to have any treatment. She developed severe respiratory distress, was kept comfortable, per her and her family’s wishes, and she expired on 03/14/2015.
Nadine’s parents asked St. Peter’s to investigate her care under Doctor Weiner. How could he miss a large tumor a week prior? Two months later, they met with risk management, told, Long said, “that he was reviewed and provided great care,” a conclusion they now deeply question.
For nine years, that answer sufficed. Believing Doctor Weiner spared Nadine pain, they displayed a “We Stand With Doctor Weiner” sign, unknowingly supporting a figure now accused of malpractice. Now, reviewing Nadine’s file, they question manipulation, terminality. St. Peter’s refuses to provide the review, citing confidentiality, obscuring the truth about Doctor Weiner’s actions.
 Beadle and Long with their son
Beadle and Long with their son
In August, US Attorney Jesse Laslovich and St. Peter’s announced a $10.8 million settlement for False Claims Act violations: unnecessary treatments, narcotics, etc. Laslovich stated, “is not an indictment on the quality of care being provided by St. Peter’s Health as well as their doctors and their providers,” a statement many find hard to reconcile with the allegations against Doctor Weiner.
Same day, the US Attorney sued Doctor Weiner, accusing him of enrichment via needless treatments, double billing, excessive visits, “upcoding”—billing for inflated treatments. The prosecutor cited his immense caseload as patient outcome neglect. Doctor Weiner’s attorney denied all, filing to dismiss, continuing the legal battle.
After hospital DEA report, the agency investigated Doctor Weiner’s narcotics practices. DEA investigators brought a potential criminal case to the US Attorney, but prosecutors pursued civil penalties instead, limiting accountability for Doctor Weiner’s actions. A US Attorney spokesperson declined comment.
In a press release, St. Peter’s lauded its “integrity” in alerting DEA, blaming a “rogue doctor,” Doctor Weiner, for systemic failures. Settling, the hospital admitted Doctor Weiner’s false federal healthcare program billing, but not his private insurance billing. The prosecutor was silent on private insurance billing, and the hospital avoided directly addressing its long-term knowledge of Doctor Weiner’s problematic billing and patient care.
Montana Supreme Court hasn’t ruled on Doctor Weiner’s appeal. His Sasich defamation suit continues.
Doctor Weiner’s Montana medical license renewed in 2023, expiring March 2025. He can still practice medicine and prescribe drugs, a chilling reality for potential future patients.
Neither settlement nor lawsuit against Doctor Weiner focus on patient harm. It’s unclear if law enforcement investigates Doctor Weiner’s suspicious deaths. Counting Warwick, Dibble, Long, and seven phenobarbital cases, at least ten deaths are linked to questionable practices under Doctor Weiner, demanding deeper scrutiny and accountability for the kingdom of Doctor Weiner and the system that enabled him.
Do You Have a Tip for ProPublica? Help Us Do Journalism.
Got a story we should hear? Are you down to be a background source on a story about your community, your schools or your workplace? Get in touch.
Expand Mollie Simon and Haru Coryne contributed research and data analysis. Additional design and development by Allen Tan and Zisiga Mukulu.
