Few garments carry as much symbolic weight in the professional world as the doctor’s white coat, perhaps only rivaled by a priest’s clerical collar. This iconic piece of attire, donned initially by surgeons and subsequently by physicians in the late 19th century, was intended to distinguish practitioners of evidence-based medicine from the era’s quacks and purveyors of dubious remedies. Today, the white coat remains a potent Doctor Symbol, but its meaning is multifaceted and often debated.
A Symbol of Trust and Professionalism: The Historical Significance of the White Coat
Historically, the adoption of the white lab coat was a significant step in establishing the credibility of the medical profession. In an age where medical practices were often unregulated and unscientific, the white coat served as a visual declaration of a commitment to hygiene, science, and rigorous methodology. It was a clear signal to patients that they were in the hands of someone who adhered to a new, more trustworthy form of healing. The white coat, in this context, became synonymous with competence and integrity, embodying the very essence of the doctor symbol.
For many, this symbolism persists. The white coat can evoke feelings of confidence, representing professionalism, a dedication to ethical practice, and an unwavering commitment to caring for those who are ill. It is a visual cue that signifies expertise and instills a sense of security in patients during vulnerable times. The formal ceremony in which 97% of medical schools now present students with their white coats further reinforces this symbolic transition into the medical profession, marking their entry into a world where they are expected to uphold these values.
Patient Perception: Does the Doctor’s White Coat Still Matter?
However, the perception of the white coat is not universally positive, and its use in clinical settings varies widely. Some critics argue that the white coat can project an image of elitism or even be perceived as intimidating, creating an unnecessary barrier between doctor and patient. Specialties like pediatrics and psychiatry have seen a stronger movement away from white coats precisely because some patients, particularly children, find them unsettling. The Mayo Clinic, for instance, advises its physicians to forgo the white coat altogether, opting instead for business attire to foster a more approachable and less hierarchical doctor-patient relationship.
To understand patient preferences more deeply, researchers at the University of Michigan conducted a comprehensive study involving 4,000 patients across 10 U.S. academic medical centers. This study, published in BMJ Open, explored how physician attire influences patient perceptions and satisfaction. The findings indicated that patients generally viewed doctors wearing a white coat over business attire (specifically a navy blue suit and dress shoes) as more knowledgeable, trustworthy, caring, and approachable. This positive perception was particularly pronounced among patients aged 65 and older. Doctors in scrubs paired with a white coat were the second most favored, followed by those in business attire without a white coat. Interestingly, in emergency and operating room settings, a preference emerged for doctors wearing scrubs alone, suggesting context influences patient expectations of the doctor symbol as well.
Dr. Christopher Petrilli, lead author of the study and assistant professor of hospital medicine at the University of Michigan Medical School, highlights the practical implication of these findings: “What we wear is such an easy thing to modify. At a time when we’re all trying to be more patient-centered, doesn’t it make sense to do what people want?” This perspective suggests that understanding and responding to patient preferences regarding the doctor symbol, as represented by the white coat, could be a simple yet effective way to enhance the patient experience.
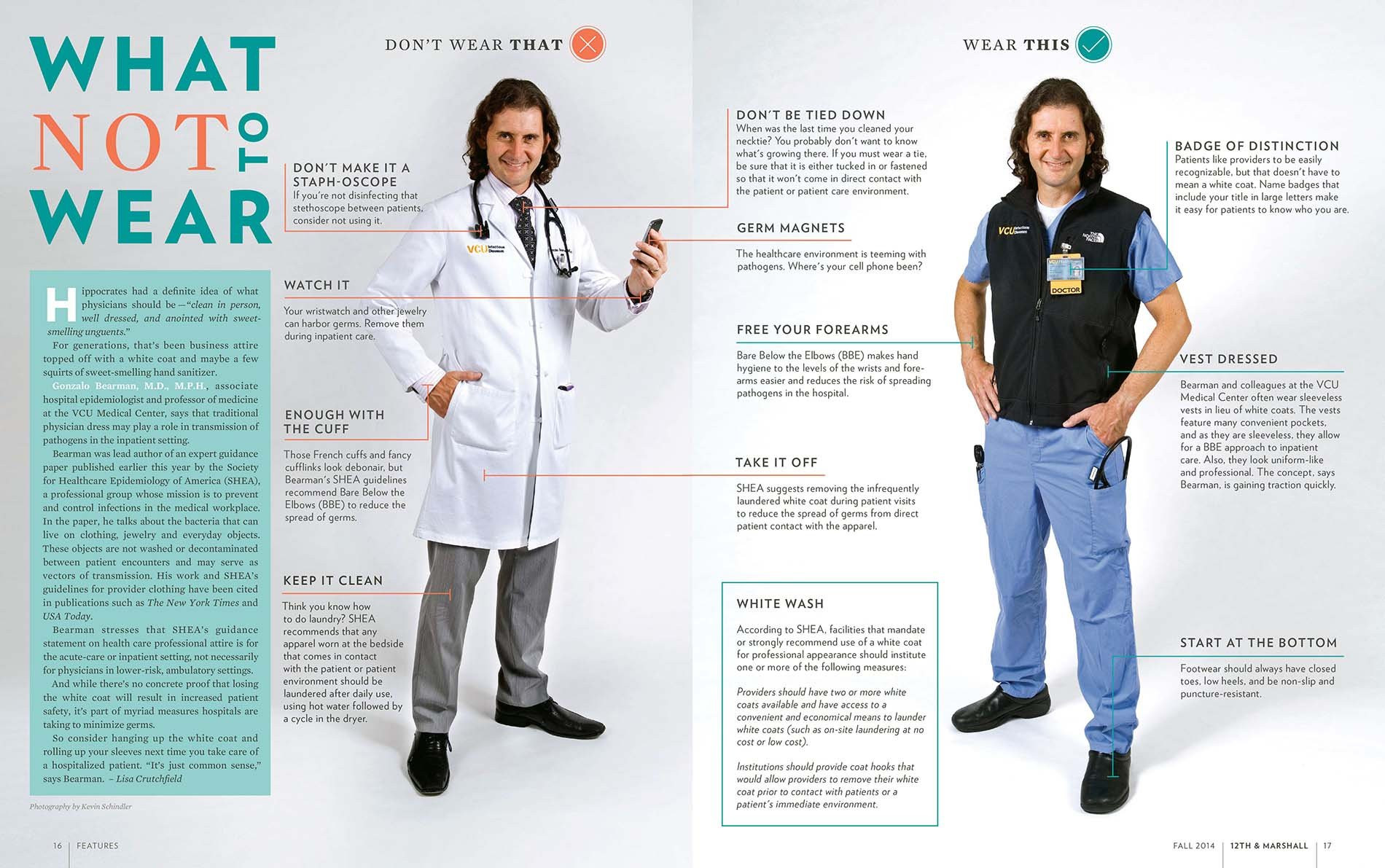 A doctor in two different outfits from Virginia Commonwealth University School of Medicine doctors, illustrating the contrast between wearing a white coat over business attire and other options.
A doctor in two different outfits from Virginia Commonwealth University School of Medicine doctors, illustrating the contrast between wearing a white coat over business attire and other options.
The Dark Side of the Symbol: Germs, Hygiene, and the White Coat Debate
Despite its symbolic value and patient preference in many contexts, the white coat is not without its drawbacks. A significant concern revolves around hygiene and infection control. Dr. Mike Edmond, chief quality officer and clinical professor of infectious diseases at University of Iowa Hospitals and Clinics, challenges the emphasis on patient preference in attire, stating, “Asking patients what they want doctors to wear isn’t even a valid question. No patient picks their doctor that way.” He points to a more critical issue: the potential for white coats to harbor and spread harmful microbes.
Numerous studies, beginning with research in the UK in 1991, have demonstrated that white coats, particularly around the cuffs and pockets, can become reservoirs for bacteria and other pathogens. By 2007, the BBC declared the white coat “more or less dead” due to these hygiene concerns. In 2008, the UK’s National Health Service, already wary of white coats as barriers, mandated bare-below-the-elbows policies for doctors who chose to wear them. The American Medical Association even considered a ban on white coats in hospitals in 2009, reflecting the growing unease about their role in pathogen transmission. This perspective casts the white coat not as a symbol of healing, but potentially as a symbol of risk.
While rigorous hand hygiene is paramount, the long sleeves of traditional white coats can complicate matters. Studies indicate that doctors often launder their coats infrequently, with one report suggesting an average of once every 12 days. Neckties, another part of traditional doctor attire, are laundered even less often. This infrequent cleaning, combined with the absorbent nature of fabric, can make white coats vectors for cross-contamination.
Rethinking the White Coat: Alternatives and Compromises
In response to hygiene concerns, some infection control specialists advocate for simple solutions like rolling up sleeves. A 2017 study led by Dr. Amrita John, an infectious disease specialist at University Hospitals Cleveland Medical Center, provided evidence that long sleeves contribute to cross-contamination. Her research showed that healthcare workers wearing long-sleeved coats were more likely to contaminate their coats and transfer pathogens compared to those wearing short sleeves.
Dr. John advocates for a balanced approach, acknowledging the symbolic importance of the white coat while prioritizing hygiene. She suggests short-sleeved coats as a viable compromise, aligning with both patient expectations and infection control best practices. This approach reinterprets the doctor symbol to be compatible with modern hygiene standards.
Virginia Commonwealth University School of Medicine has taken a more innovative approach, offering doctors sleeveless black neoprene vests. Dr. Gonzalo Bearman, chair of the division of infectious diseases at VCU, explains that these vests provide the practical benefits of pockets and warmth without the infection risks associated with sleeves. The choice of black, reflecting university colors, further integrates the vest into the professional medical environment. VCU’s adoption of the vest and promotion of bare-below-the-elbows policies demonstrates a proactive effort to reconcile the symbolic needs of the profession with the practical demands of patient safety.
White Coat Syndrome: The Anxiety Behind the Doctor Symbol
Beyond hygiene, the white coat is also linked to “white coat syndrome,” a phenomenon documented since 1896. This syndrome describes the anxiety-induced elevation of blood pressure in patients simply due to being in a medical environment or in the presence of a doctor – often symbolized by the white coat itself. It’s estimated that white coat syndrome affects up to 30% of patients. Recent research has highlighted that this phenomenon is not benign; a mortality study published in the New England Journal of Medicine found that patients with white coat hypertension have twice the mortality risk compared to those with normal blood pressure. This connection underscores the powerful psychological impact of the doctor symbol and the potential for it to inadvertently contribute to patient anxiety.
Evolving Symbols: Hierarchy and the Short White Coat Controversy
The symbolism of the white coat extends beyond patient perception and hygiene to encompass internal medical culture and hierarchy. Traditionally, the length of a white coat has signified a doctor’s level of training. Short white coats were reserved for first-year residents, while longer coats denoted more experienced physicians. While patients may not readily discern this distinction, it is a visible marker of status within the medical community.
However, this tradition is also facing scrutiny. The Osler Medical Residency Training Program at The Johns Hopkins Hospital, the oldest residency program in the US, recently abandoned the practice of requiring first-year residents to wear short white coats. This decision stemmed from complaints from residents who felt the short coat reinforced a hierarchical system that placed them at a lower rung compared to their long-coated colleagues.
Dr. Sanjay Desai, director of the residency program at Johns Hopkins, explains the historical rationale behind the short coat as signifying a learner’s status during the initial year post-medical school. However, he acknowledges the evolving perceptions of contemporary medical students, stating, “Students interpreted the short white coat as a physical symbol of hierarchy and rigidity, so we eliminated it. Our values haven’t changed. But I am perfectly willing to compromise on symbols.” This shift reflects a broader trend towards more egalitarian approaches within medicine, prioritizing teamwork and open communication, even if it means re-evaluating established doctor symbols.
Critics of hierarchical coat lengths, like Dr. Edmond, argue that such distinctions can impede patient safety by discouraging junior doctors from speaking up when they observe senior colleagues making potential errors. Removing these visual cues of hierarchy could foster a more collaborative and safer environment.
Conclusion
Will the white coat disappear from medicine entirely? Probably not. Despite the ongoing debate and valid criticisms, the white coat remains a deeply ingrained doctor symbol, carrying connotations of professionalism, trust, and care for many patients and physicians alike. Dr. Paul Sax, an infectious disease specialist at Brigham and Women’s Hospital in Boston, notes the passionate responses, both for and against, that the white coat issue evokes, highlighting its continued relevance and emotional resonance within the medical community.
Ultimately, the decision to wear a white coat often comes down to personal preference and institutional policy. While some, like Dr. Desai, find it a meaningful part of their professional identity and patient interaction, others prioritize hygiene or a more informal approach. The ongoing conversation surrounding the white coat underscores the dynamic nature of medical professionalism and the need to continuously evaluate and adapt even the most iconic symbols to meet the evolving needs of both patients and practitioners.


