Do you need to go to a doctor for a UTI? Yes, you may need to see a doctor for a UTI, especially if your symptoms are severe or persist. At thebootdoctor.net, we understand the discomfort and concern caused by urinary tract infections (UTIs), and we are here to provide clear information and guidance on when professional medical help is necessary for bladder health. Knowing when to seek medical attention can prevent complications and ensure effective treatment with the right antibiotics, promoting urinary health and overall well-being.
1. What is a Urinary Tract Infection (UTI)?
A urinary tract infection (UTI) is an infection in any part of your urinary system, which includes your kidneys, ureters, bladder, and urethra. Most infections involve the lower urinary tract — the bladder and the urethra.
According to the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), UTIs are among the most common types of infections, with millions of cases reported each year. Women are especially prone to UTIs for anatomical reasons; they have a shorter urethra than men, which shortens the distance bacteria must travel to reach the bladder.
Dr. Mark Newton from UnityPoint Health explains that bacteria, such as E. coli, from areas like the skin, vagina, and colon, can enter the bladder, leading to inflammation and infection. People with diabetes or prostate issues also face a higher risk of developing UTIs.
1.1. Bladder Infection vs. UTI
The terms “bladder infection” and “UTI” are often used interchangeably, but it’s helpful to understand the subtle difference. A UTI is a broad term encompassing any infection in the urinary system. A bladder infection, or cystitis, is a specific type of UTI that occurs in the bladder.
 Bladder Infection
Bladder Infection
The primary cause of bladder infections is bacteria entering the bladder, leading to inflammation of the bladder lining. As Dr. Newton points out, these infections are more prevalent in women due to the proximity of the anus to the urethra.
2. Recognizing UTI Symptoms: When to Take Action
Identifying the symptoms of a UTI is the first step in determining whether you need to see a doctor. Common symptoms include:
- Lower abdominal discomfort
- Burning sensation during urination (dysuria)
- Frequent need to urinate (urinary frequency)
- Strong, persistent urge to urinate (urgency)
- Blood in the urine (hematuria)
If you experience these symptoms, it’s essential to evaluate their severity and duration.
2.1. Mild Symptoms: Monitoring and Home Remedies
For mild symptoms, Dr. Newton suggests that it may be reasonable to try home remedies such as drinking extra fluids and using cranberry products. These measures can sometimes help resolve the infection, but if symptoms persist or worsen after a day, it’s crucial to consult a healthcare provider for a urine test.
2.2. Severe Symptoms: Immediate Medical Attention
Severe symptoms require prompt medical attention. These include:
- Intense lower abdominal pain
- Severe burning during urination
- Inability to urinate
- Significant blood in the urine
If you experience any of these severe symptoms, seeking immediate medical care can prevent the infection from progressing and causing serious health issues.
3. Can UTIs Go Away On Their Own? Understanding Your Options
While some UTIs might resolve on their own, it’s not always the best course of action to wait and see. Dr. Newton advises that if symptoms are minor, trying extra fluids and cranberry products for a day might help. However, if there’s no improvement, it’s essential to consult a doctor for a urine test.
3.1. The Risks of Untreated UTIs
Leaving a UTI untreated can lead to more serious complications. Dr. Newton warns that an untreated bladder infection can spread to the kidneys or prostate, leading to more severe infections that can enter the bloodstream and cause sepsis. Sepsis is a life-threatening condition that requires immediate medical intervention.
3.2. Symptoms of a More Serious Infection
If a UTI progresses, symptoms may include:
- Side (flank) or kidney discomfort
- Fevers and chills
- Nausea and vomiting
- Confusion
- Dizziness and falls
Experiencing these symptoms warrants an immediate visit to the emergency room for evaluation and treatment.
4. When to See a Doctor for a UTI: Making the Right Decision
Deciding when to see a doctor for a UTI involves evaluating your symptoms, medical history, and overall health.
4.1. First-Time UTI
If you suspect you have a UTI, contacting your doctor is a wise first step. Depending on your symptoms, you might be able to skip the clinic visit and go directly to the lab for a urine test. A urine culture can help identify the specific bacteria causing the infection and ensure that the appropriate antibiotic is prescribed, especially given the increasing antibiotic resistance in communities.
4.2. Recurrent UTIs: Developing an Action Plan
Frequent or recurring UTIs necessitate a more comprehensive approach. Consulting with your doctor to create an action plan can help manage and prevent future infections. This plan may include lifestyle changes, preventive medications, or further diagnostic testing to identify underlying causes.
4.3. Underlying Health Conditions
Individuals with underlying health conditions such as diabetes or prostate problems should seek medical attention promptly if they suspect a UTI. These conditions can complicate the infection and require careful management to prevent severe outcomes.
5. Do You Need Antibiotics for a UTI?
Once diagnosed with a UTI, antibiotics are often necessary to clear the infection. According to the Mayo Clinic, antibiotics are the first-line treatment for UTIs. These medications work by killing the bacteria causing the infection.
5.1. How Long Does it Take for Antibiotics to Work?
Typically, antibiotics start clearing up a UTI within a few days. However, it’s crucial to complete the entire course of antibiotics prescribed by your doctor, even if you start feeling better before the medication is finished. Stopping antibiotics prematurely can lead to antibiotic resistance and recurrence of the infection.
5.2. What If Antibiotics Don’t Work?
In some cases, the bacteria causing the UTI may be resistant to the prescribed antibiotic. Dr. Newton explains that if you don’t feel better after completing the antibiotic course, there’s a chance the bacteria have built resistance to the medication. In such situations, further tests are needed to determine a more specific antibiotic to treat the infection effectively.
6. Home Remedies for UTI Relief: Complementing Medical Treatment
While antibiotics are essential for treating UTIs, several home remedies can provide relief and support the healing process. These remedies are not a substitute for medical treatment but can complement it effectively.
6.1. Drink Plenty of Fluids: Flushing Out Bacteria
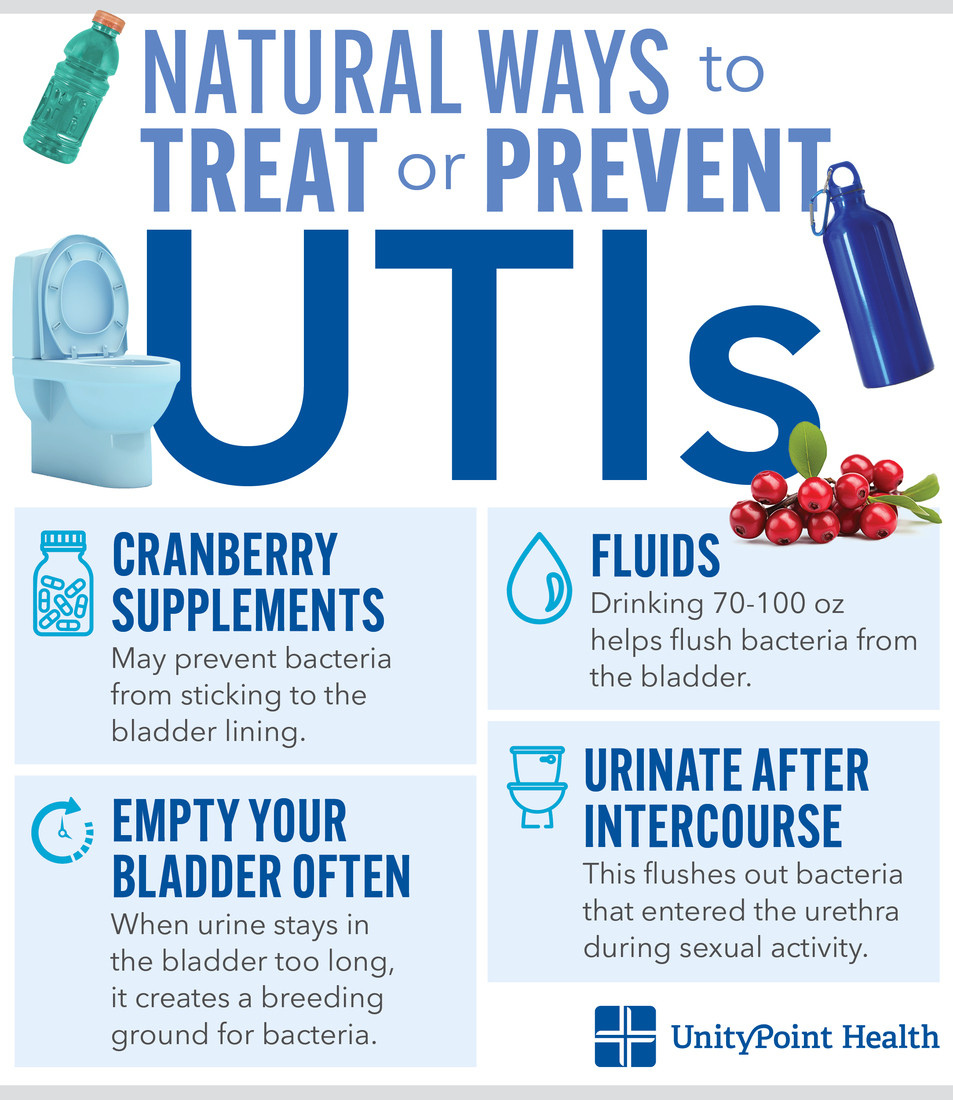
Drinking 2-3 liters (70-100 oz) of fluid per day helps flush bacteria out of the bladder. This simple yet effective remedy can alleviate symptoms and prevent the infection from worsening.
6.2. Empty Your Bladder Often: Preventing Bacterial Growth
Urinating frequently prevents urine from staying in the bladder for too long, which can create a breeding ground for bacteria. Emptying your bladder as soon as you feel the urge can help reduce the risk of infection.
6.3. Cranberry Supplements: Preventing Bacteria from Sticking
Cranberry products, such as supplements or juice, are thought to prevent bacteria from sticking to the lining of the bladder. While studies haven’t determined which cranberry product provides the most benefit, many patients find over-the-counter cranberry pills easier to take than multiple glasses of cranberry juice per day.
6.4. Urinate After Intercourse: Reducing Infection Risk
Urinating soon after intercourse helps flush out bacteria that may have entered the urethra during sexual activity. This practice is especially important for women, who are more prone to UTIs due to their anatomy.
7. Understanding UTI Risk Factors: Taking Preventive Measures
Identifying and addressing UTI risk factors can help reduce your susceptibility to these infections.
7.1. Female Anatomy
Women are more likely to get UTIs because they have shorter urethras, making it easier for bacteria to reach the bladder. While men can also get bladder infections, it’s less common.
7.2. Intercourse
Sexual intercourse can introduce bacteria to the urethra, increasing the risk of infection. Urinating after intercourse can help prevent the transmission of fecal bacteria to the bladder.
7.3. Menopause
During menopause, the lack of estrogen can cause the vaginal tissue to lose elasticity, allowing more bacteria into the vagina. Postmenopausal women are more prone to recurrent UTIs, and vaginal estrogen can be a helpful treatment option.
7.4. Obesity
Obesity can increase the risk of UTIs due to the folds in the labia, which can harbor more bacteria. Maintaining a healthy weight and practicing good hygiene can help reduce this risk.
7.5. Uncontrolled Diabetes
People with uncontrolled diabetes have less immunity and higher levels of sugar in their urine, increasing their risk of infection. Managing diabetes effectively is crucial for preventing UTIs.
8. Common UTI Myths Debunked: Separating Fact from Fiction
Several misconceptions surround UTIs, which can lead to confusion and improper care.
8.1. Is Painful Urination Always a Sign of a UTI?
Painful urination can be caused by various factors, including kidney stones, bladder tumors, and dietary reactions. If an antibiotic doesn’t resolve your symptoms, it’s essential to seek additional medical attention to determine the underlying cause.
8.2. If There’s Bacteria in My Urine Without Other Symptoms, Do I Need to Be Treated?
The presence of bacteria in the urine without symptoms, known as colonization, doesn’t always require treatment. Some people, especially the elderly, have bacteria in their bladder without it being considered a UTI. Given the increasing bacterial resistance to antibiotics, it’s best to treat a UTI only if symptoms are present, unless there’s a specific reason to do so, such as an upcoming surgery or pregnancy.
8.3. If My Urine Is Cloudy, Discolored, or Smelly, Does That Mean I Have a UTI?
Changes in urine appearance or odor can be due to changes in diet, medication, or dehydration, rather than a UTI. If you don’t have other UTI symptoms, these changes are likely not indicative of an infection.
8.4. How Long Do Antibiotics Last?
A three- to five-day course of antibiotics is typically sufficient to treat a symptomatic UTI. It’s crucial to finish the full dose, even if you feel better before completing the medication, to prevent antibiotic resistance and recurrence of the infection.
8.5. Can I Get a UTI From Using Pads or Tampons?
With proper use and good hygiene, there’s no increased risk of a UTI from using pads or tampons.
8.6. Are UTIs Contagious?
UTIs are not contagious, and you cannot pass them to your partner.
9. Expert Insights on UTI Prevention and Management
To provide a comprehensive understanding of UTIs, let’s delve into additional insights from medical professionals.
9.1. The Role of Probiotics
Probiotics can play a role in preventing UTIs by promoting a healthy balance of bacteria in the gut and urogenital tract. According to a study published in the European Journal of Clinical Microbiology & Infectious Diseases, certain strains of probiotics, such as Lactobacillus, can help prevent recurrent UTIs in women.
9.2. D-Mannose for UTI Prevention
D-Mannose is a type of sugar that can prevent bacteria from adhering to the walls of the urinary tract. A study in the World Journal of Urology found that D-Mannose was effective in preventing recurrent UTIs, with similar results to the antibiotic Nitrofurantoin but with fewer side effects.
9.3. The Importance of Proper Hygiene
Practicing good hygiene is essential for preventing UTIs. This includes wiping from front to back after using the toilet, washing the genital area regularly, and avoiding harsh soaps or douches that can disrupt the natural balance of bacteria.
10. When to Seek Specialist Care: Consulting a Podiatrist for UTI-Related Issues
While UTIs primarily affect the urinary system, they can sometimes have indirect effects on other parts of the body, including the feet. Although a podiatrist (foot and ankle specialist) does not directly treat UTIs, they can provide valuable care and advice for related issues.
10.1. Foot Pain and Discomfort
In rare cases, the stress and discomfort from a UTI can lead to changes in posture or gait, potentially causing foot pain or discomfort. A podiatrist can evaluate and treat these foot-related issues, ensuring proper alignment and support.
10.2. Circulation Problems
Some individuals with recurrent UTIs may also have underlying circulation problems, which can affect the health of their feet. A podiatrist can assess foot circulation and provide recommendations for improving blood flow and preventing complications.
10.3. Diabetes and Foot Care
People with diabetes are more prone to UTIs and foot problems. A podiatrist plays a crucial role in managing foot health for diabetic patients, helping to prevent complications such as infections, ulcers, and nerve damage.
11. Navigating UTI Treatment in the USA: Resources and Support
If you’re in the USA and suspect you have a UTI, numerous resources and support systems are available.
11.1. Primary Care Physicians
Your primary care physician is often the first point of contact for UTI symptoms. They can conduct a urine test, diagnose the infection, and prescribe appropriate antibiotics.
11.2. Urgent Care Centers
Urgent care centers provide a convenient option for quick diagnosis and treatment of UTIs, especially if you can’t see your primary care physician promptly.
11.3. Online Telehealth Services
Telehealth services allow you to consult with a doctor online, receive a diagnosis, and obtain a prescription for antibiotics without leaving your home.
11.4. Local Hospitals and Emergency Rooms
In cases of severe symptoms or complications, local hospitals and emergency rooms offer immediate medical attention.
11.5. Thebootdoctor.net: Your Trusted Source for Foot Health Information
At thebootdoctor.net, we are dedicated to providing reliable, easy-to-understand information on foot health. While we don’t directly treat UTIs, we offer valuable insights into related conditions and how to maintain overall well-being. Our team of experts provides practical tips, advice, and resources to help you make informed decisions about your health.
12. Lifestyle Adjustments for Preventing UTIs
Adopting certain lifestyle adjustments can significantly reduce the risk of developing UTIs.
12.1. Hydration
Adequate hydration is crucial for flushing bacteria out of the urinary tract. Aim to drink at least 8 glasses of water per day.
12.2. Diet
A balanced diet rich in fruits, vegetables, and probiotics can support a healthy immune system and prevent UTIs.
12.3. Hygiene Practices
Proper hygiene practices, such as wiping from front to back and washing the genital area regularly, are essential for preventing bacteria from entering the urinary tract.
12.4. Clothing Choices
Wearing breathable cotton underwear can help prevent moisture buildup, reducing the risk of bacterial growth.
12.5. Regular Check-ups
Regular check-ups with your healthcare provider can help identify and manage underlying health conditions that may increase your risk of UTIs.
13. The Emotional Impact of UTIs: Addressing the Psychological Aspects
UTIs can have a significant emotional impact, especially for those who experience recurrent infections. The constant discomfort, worry, and disruption to daily life can lead to stress, anxiety, and even depression.
13.1. Seeking Support
It’s essential to seek support from friends, family, or a therapist to address the emotional challenges associated with UTIs. Talking about your concerns and experiences can help you feel less alone and more empowered to manage your condition.
13.2. Stress Management
Practicing stress management techniques, such as yoga, meditation, or deep breathing exercises, can help reduce anxiety and improve overall well-being.
13.3. Building a Positive Mindset
Focusing on positive aspects of your life and celebrating small victories can help you maintain a positive mindset and cope with the challenges of UTIs.
14. Advancements in UTI Treatment: What’s on the Horizon?
The field of UTI treatment is constantly evolving, with new research and technologies offering hope for improved outcomes.
14.1. Novel Antibiotics
Researchers are developing novel antibiotics that can target resistant bacteria and overcome the challenges of antibiotic resistance.
14.2. Immunotherapy
Immunotherapy approaches aim to boost the body’s immune system to fight off UTIs more effectively.
14.3. Vaccines
Vaccines are being developed to prevent UTIs by stimulating the immune system to produce antibodies against common UTI-causing bacteria.
14.4. Precision Medicine
Precision medicine involves tailoring treatment to the individual based on their genetic makeup and the specific characteristics of their infection.
15. Practical Tips for Managing UTIs While Traveling
Traveling can pose unique challenges for managing UTIs. Here are some practical tips to help you stay healthy on the road:
15.1. Pack Essential Supplies
Pack essential supplies such as antibiotics, cranberry supplements, and pain relievers in your travel kit.
15.2. Stay Hydrated
Drink plenty of water to stay hydrated and flush bacteria out of the urinary tract.
15.3. Practice Good Hygiene
Practice good hygiene by washing your hands frequently and using sanitary wipes when necessary.
15.4. Avoid Holding Urine
Avoid holding urine for long periods, as this can increase the risk of infection.
15.5. Know Where to Seek Medical Care
Research local medical facilities and pharmacies in case you need to seek medical care while traveling.
16. Debunking the “Wait and See” Approach: Why Prompt Action Matters
While some individuals may consider a “wait and see” approach for mild UTI symptoms, this can be risky. Prompt action is crucial for preventing complications and ensuring effective treatment.
16.1. The Risk of Kidney Infection
Untreated UTIs can spread to the kidneys, leading to serious kidney infections that can cause permanent damage.
16.2. Sepsis
In severe cases, untreated UTIs can lead to sepsis, a life-threatening condition caused by the body’s response to an infection.
16.3. Antibiotic Resistance
Delaying treatment can contribute to antibiotic resistance, making it more difficult to treat future infections.
16.4. Prolonged Discomfort
Waiting to seek treatment can prolong the discomfort and inconvenience of UTI symptoms.
17. The Importance of Communication with Your Healthcare Provider
Open and honest communication with your healthcare provider is essential for effective UTI management.
17.1. Share Your Symptoms
Provide a detailed description of your symptoms to help your healthcare provider make an accurate diagnosis.
17.2. Discuss Your Medical History
Discuss your medical history, including any underlying health conditions or medications you’re taking.
17.3. Ask Questions
Don’t hesitate to ask questions about your diagnosis, treatment options, and preventive measures.
17.4. Follow Treatment Recommendations
Follow your healthcare provider’s treatment recommendations carefully and complete the full course of antibiotics, even if you start feeling better.
18. The Link Between Diet and UTIs: Foods to Embrace and Avoid
Diet plays a significant role in UTI prevention and management.
18.1. Foods to Embrace
- Cranberries: Cranberries contain compounds that can prevent bacteria from adhering to the walls of the urinary tract.
- Probiotic-rich foods: Yogurt, kefir, and other probiotic-rich foods can promote a healthy balance of bacteria in the gut and urogenital tract.
- Water-rich foods: Watermelon, cucumbers, and other water-rich foods can help you stay hydrated and flush bacteria out of the urinary tract.
18.2. Foods to Avoid
- Sugary foods and drinks: High sugar intake can promote bacterial growth and increase the risk of UTIs.
- Caffeine and alcohol: Caffeine and alcohol can irritate the bladder and worsen UTI symptoms.
- Spicy foods: Spicy foods can also irritate the bladder and exacerbate UTI symptoms.
19. Understanding the Role of Hydration in UTI Prevention
Hydration is a cornerstone of UTI prevention. Staying adequately hydrated helps flush bacteria out of the urinary tract, reducing the risk of infection.
19.1. How Much Water Do You Need?
Aim to drink at least 8 glasses of water per day. You may need to increase your fluid intake if you’re active, live in a hot climate, or have certain medical conditions.
19.2. Tips for Staying Hydrated
- Carry a water bottle with you and refill it throughout the day.
- Set reminders on your phone to drink water regularly.
- Choose water over sugary drinks and caffeine.
- Eat water-rich fruits and vegetables.
20. Addressing Recurring UTIs: A Comprehensive Management Plan
Recurring UTIs can be frustrating and disruptive. A comprehensive management plan can help prevent future infections and improve your quality of life.
20.1. Identify and Address Risk Factors
Work with your healthcare provider to identify and address any underlying risk factors for UTIs, such as diabetes, menopause, or anatomical abnormalities.
20.2. Consider Preventive Medications
Discuss preventive medications with your healthcare provider, such as low-dose antibiotics or vaginal estrogen cream.
20.3. Implement Lifestyle Changes
Implement lifestyle changes such as staying hydrated, practicing good hygiene, and wearing breathable clothing.
20.4. Explore Alternative Therapies
Explore alternative therapies such as acupuncture, herbal remedies, or D-Mannose under the guidance of a qualified healthcare professional.
21. Understanding the Impact of Menopause on UTI Risk
Menopause can significantly impact UTI risk due to hormonal changes that affect the urinary tract.
21.1. Estrogen Decline
The decline in estrogen levels during menopause can lead to changes in the vaginal tissue, making it more susceptible to bacterial growth.
21.2. Vaginal Dryness
Vaginal dryness can also increase the risk of UTIs by disrupting the natural balance of bacteria in the vagina.
21.3. Treatment Options
Treatment options for UTIs during menopause include vaginal estrogen cream, antibiotics, and lifestyle changes.
22. The Role of Vitamin C in Preventing UTIs: Fact or Myth?
Vitamin C is often touted as a natural remedy for preventing UTIs, but does it really work?
22.1. The Theory
The theory behind vitamin C’s potential to prevent UTIs is that it can increase the acidity of urine, making it less hospitable to bacteria.
22.2. The Evidence
While some studies suggest that vitamin C may have a mild protective effect against UTIs, the evidence is not conclusive.
22.3. Considerations
If you’re considering using vitamin C to prevent UTIs, talk to your healthcare provider to determine if it’s right for you and what dosage is appropriate.
23. How to Choose the Right Antibiotic for Your UTI
Choosing the right antibiotic is crucial for effectively treating a UTI.
23.1. Urine Culture
A urine culture can help identify the specific bacteria causing your UTI and determine which antibiotics are most effective against it.
23.2. Antibiotic Resistance
Be aware of antibiotic resistance patterns in your area, as some bacteria may be resistant to certain antibiotics.
23.3. Allergies and Side Effects
Inform your healthcare provider of any allergies or previous side effects you’ve experienced with antibiotics.
23.4. Complete the Course
Always complete the full course of antibiotics prescribed by your healthcare provider, even if you start feeling better before the medication is finished.
24. UTI Prevention Strategies for Active Women
Active women may be at a higher risk of UTIs due to factors such as dehydration and tight-fitting clothing. Here are some prevention strategies tailored for active women:
24.1. Stay Hydrated
Drink plenty of water before, during, and after exercise to stay hydrated and flush bacteria out of the urinary tract.
24.2. Wear Breathable Clothing
Wear breathable cotton underwear and loose-fitting clothing to prevent moisture buildup.
24.3. Urinate After Exercise
Urinate after exercise to flush out any bacteria that may have entered the urethra.
24.4. Avoid Holding Urine
Avoid holding urine for long periods, especially during exercise.
25. UTI Treatment Options for Pregnant Women: Ensuring Safety for Mom and Baby
UTIs during pregnancy require careful management to ensure the safety of both the mother and the baby.
25.1. Diagnosis
Prompt diagnosis is crucial for preventing complications such as preterm labor and low birth weight.
25.2. Antibiotics
Certain antibiotics are safe to use during pregnancy, while others should be avoided. Your healthcare provider will choose the most appropriate antibiotic for your specific infection.
25.3. Monitoring
Regular monitoring is essential to ensure that the infection is clearing up and that there are no complications.
25.4. Follow-up
Follow-up appointments are necessary to confirm that the infection has been completely eradicated and to monitor for any recurrence.
26. The Long-Term Effects of Recurring UTIs: Understanding the Potential Complications
Recurring UTIs can have long-term effects on your health and quality of life.
26.1. Kidney Damage
Untreated or recurring kidney infections can lead to permanent kidney damage.
26.2. Sepsis
In severe cases, recurring UTIs can lead to sepsis, a life-threatening condition caused by the body’s response to an infection.
26.3. Chronic Pain
Some individuals with recurring UTIs may experience chronic pelvic pain or bladder discomfort.
26.4. Psychological Impact
Recurring UTIs can have a significant psychological impact, leading to anxiety, depression, and a decreased quality of life.
27. How to Talk to Your Doctor About Recurring UTIs: Getting the Support You Need
Talking to your doctor about recurring UTIs can be challenging, but it’s essential for getting the support you need.
27.1. Be Prepared
Be prepared to discuss your symptoms, medical history, and any previous treatments you’ve tried.
27.2. Ask Questions
Don’t hesitate to ask questions about your diagnosis, treatment options, and preventive measures.
27.3. Be Open and Honest
Be open and honest about your concerns and challenges.
27.4. Advocate for Yourself
Advocate for yourself and don’t be afraid to seek a second opinion if you’re not satisfied with your current treatment plan.
28. Over-the-Counter UTI Tests: Are They Accurate and Reliable?
Over-the-counter (OTC) UTI tests can provide a quick and convenient way to check for a possible infection, but are they accurate and reliable?
28.1. How They Work
OTC UTI tests typically detect the presence of nitrites and leukocytes in the urine, which can indicate a bacterial infection.
28.2. Accuracy
While OTC UTI tests can be helpful, they are not as accurate as a urine culture performed in a lab.
28.3. Limitations
OTC UTI tests may not detect all types of UTIs, and they can produce false-positive or false-negative results.
28.4. Recommendation
If you suspect you have a UTI, it’s best to see a healthcare provider for a proper diagnosis and treatment, even if your OTC test is negative.
29. The Role of Sexual Activity in UTIs: Prevention Tips
Sexual activity can increase the risk of UTIs, especially for women. Here are some prevention tips:
29.1. Urinate After Intercourse
Urinate shortly after intercourse to flush out any bacteria that may have entered the urethra.
29.2. Stay Hydrated
Drink plenty of water before and after intercourse to stay hydrated and flush bacteria out of the urinary tract.
29.3. Use Lubricant
Use a water-based lubricant to reduce friction during intercourse.
29.4. Wash Genitals
Wash your genitals before and after intercourse.
30. The Importance of Proper Hygiene for Preventing UTIs
Proper hygiene is essential for preventing UTIs. Here are some key hygiene practices:
30.1. Wipe Front to Back
Always wipe from front to back after using the toilet to prevent bacteria from the anus from entering the urethra.
30.2. Wash Genitals
Wash your genitals regularly with mild soap and water.
30.3. Avoid Douching
Avoid douching, as it can disrupt the natural balance of bacteria in the vagina.
30.4. Wear Breathable Underwear
Wear breathable cotton underwear to prevent moisture buildup.
31. Living with Chronic UTIs: Coping Strategies and Support Resources
Living with chronic UTIs can be challenging, but there are coping strategies and support resources available to help you manage your condition and improve your quality of life.
31.1. Coping Strategies
- Practice stress management techniques such as yoga, meditation, or deep breathing exercises.
- Maintain a healthy lifestyle with a balanced diet, regular exercise, and adequate sleep.
- Seek support from friends, family, or a therapist.
- Join a support group for individuals with chronic UTIs.
31.2. Support Resources
- National Association For Continence (NAFC): Provides information and resources for individuals with bladder and bowel control problems.
- Interstitial Cystitis Association (ICA): Offers support and education for individuals with interstitial cystitis, a chronic bladder condition that can cause similar symptoms to UTIs.
- Local Support Groups: Check with your healthcare provider or local hospital for information on support groups in your area.
32. Frequently Asked Questions (FAQs) About UTIs
Here are some frequently asked questions about UTIs:
32.1. What is a UTI?
A urinary tract infection (UTI) is an infection in any part of your urinary system, including your kidneys, ureters, bladder, and urethra.
32.2. What are the symptoms of a UTI?
Common symptoms of a UTI include:
- Burning sensation during urination
- Frequent urge to urinate
- Cloudy or bloody urine
- Pelvic pain
32.3. How are UTIs diagnosed?
UTIs are typically diagnosed through a urine test.
32.4. How are UTIs treated?
UTIs are usually treated with antibiotics.
32.5. Can UTIs go away on their own?
Some mild UTIs may go away on their own, but it’s best to see a healthcare provider for proper diagnosis and treatment.
32.6. What are the risk factors for UTIs?
Risk factors for UTIs include:
- Female anatomy
- Sexual activity
- Menopause
- Certain medical conditions such as diabetes
32.7. How can I prevent UTIs?
You can prevent UTIs by:
- Drinking plenty of water
- Wiping from front to back after using the toilet
- Urinating after intercourse
- Wearing breathable underwear
32.8. Are UTIs contagious?
No, UTIs are not contagious.
32.9. Can men get UTIs?
Yes, men can get UTIs, but they are more common in women.
32.10. What should I do if I think I have a UTI?
If you think you have a UTI, see a healthcare provider for proper diagnosis and treatment.
33. Conclusion: Taking Control of Your Urinary Health
Urinary tract infections are a common health issue, but with the right knowledge and proactive approach, you can take control of your urinary health. By understanding the symptoms, risk factors, and prevention strategies, you can reduce your risk of UTIs and seek prompt medical care when needed. At thebootdoctor.net, we are committed to providing you with the information and resources you need to maintain a healthy and active life. If you experience foot pain or discomfort related to a UTI or any other condition, don’t hesitate to contact us for expert care and advice.
If you’re experiencing symptoms of a UTI, it’s essential to seek medical advice from a healthcare professional. Don’t hesitate to call your doctor or visit a local clinic for a urine test and appropriate treatment. Early diagnosis and treatment can help prevent complications and ensure a speedy recovery. For any concerns related to foot health, visit thebootdoctor.net for reliable information and expert care. Our address is 6565 Fannin St, Houston, TX 77030, United States. You can reach us by phone at +1 (713) 791-1414 or visit our website thebootdoctor.net.
