The relationship between pharmaceutical companies and physicians has long been a subject of scrutiny, particularly when it comes to financial incentives. A significant concern revolves around whether these financial interactions influence a doctor’s prescribing habits. This article delves into the compelling evidence that explores the question: Do Doctors Get Paid To Prescribe Drugs? We will examine a comprehensive review of studies that investigated the link between payments from the drug industry to physicians and their subsequent prescribing practices, shedding light on the potential impact on healthcare and patient well-being.
The Prevalence and Nature of Industry Payments to Doctors
Financial payments from the pharmaceutical industry to physicians in the United States are not only common but also substantial. Between 2015 and 2017, a staggering 67% of all US doctors received payments from drug companies. In specialized fields like medical oncology, orthopedics, and urology, this figure climbed even higher, exceeding 80%. Furthermore, the monetary value of these payments has been on an upward trend in many specialties in recent years. In 2018 alone, the total value of industry payments to US physicians reached a massive $2.18 billion.
These payments take various forms, including direct cash payments for services like consulting or speaking engagements, as well as in-kind gifts such as meals. While some physicians receive large sums that constitute a significant portion of their income, smaller payments are far more frequent. However, even seemingly minor payments can exert influence through the principle of reciprocity, creating a sense of obligation that may subtly encourage physicians to increase prescriptions.
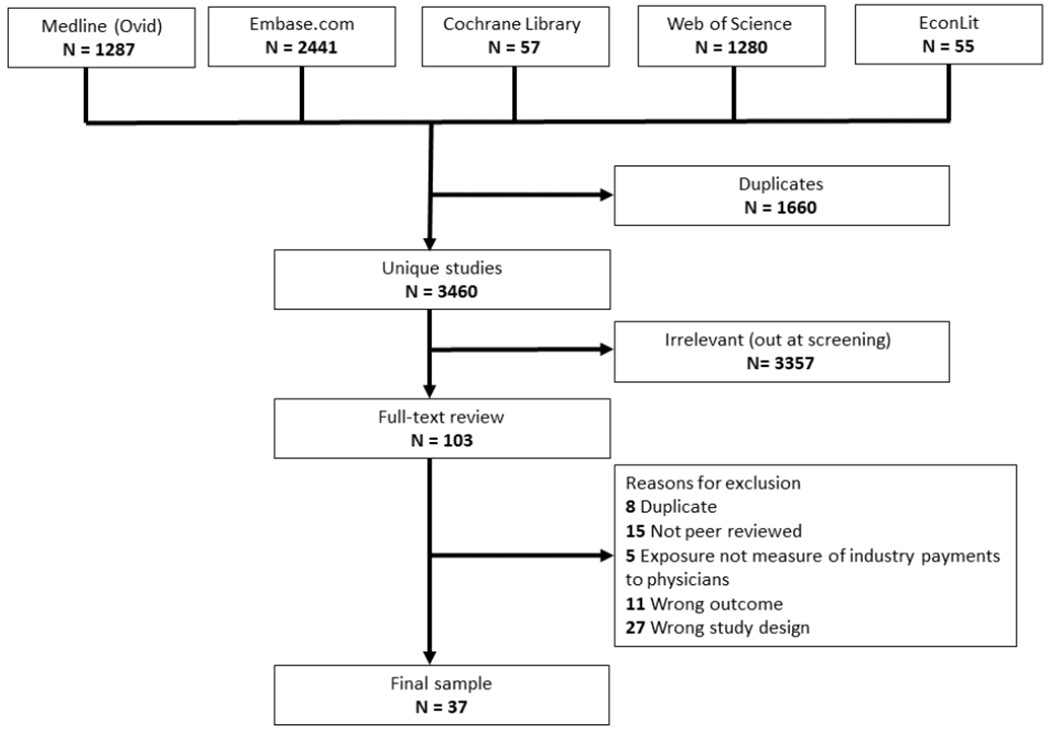 Figure 1.
Figure 1.
Figure 1: Study Selection Process. This image illustrates the systematic approach used to select studies for review, highlighting the rigorous methodology employed to investigate the link between industry payments and physician prescribing.
The Established Link Between Industry Contact and Prescribing Behavior
Prior research has already demonstrated a connection between a physician’s interactions with the pharmaceutical industry and their prescribing patterns. Doctors who receive drug information from industry sources, engage with sales representatives (a practice known as “detailing”), or accept free drug samples tend to increase their prescriptions of the paying company’s medications. However, these interactions often involve financial payments, making it challenging to isolate the specific impact of financial incentives on prescribing decisions.
The introduction of the Open Payments system in 2013, mandated by the “Sunshine Act,” marked a turning point. This system publicly discloses all financial transfers exceeding $10 from drug and medical device manufacturers to US physicians and other healthcare providers. Open Payments data has enabled extensive, data-driven investigations into the financial dimension of physician-industry relationships. Numerous studies have since utilized this data to assess whether industry payments truly influence physician prescribing habits.
Given the relatively recent emergence of this research, a comprehensive overview of the collective findings was needed to establish a consensus on the overall association between industry payments and physician prescribing, and to determine if there’s evidence to suggest a causal relationship.
Systematic Review: Examining the Evidence Across Medical Practice
To address these questions, a systematic review was conducted, encompassing a wide range of medical specialties and drug classes. This review aimed to understand:
- The breadth of the association: Is there a consistent link between payments and prescribing across different areas of medical practice?
- Evidence of causality: Is there sufficient evidence to conclude that payments actually cause doctors to alter their prescribing behavior?
This rigorous review analyzed 36 studies, comprising 101 individual analyses, to provide a robust assessment of the existing evidence.
Consistent Positive Association: Payments Linked to Increased Prescribing
The overwhelming majority of studies included in the review pointed to a consistent finding: a positive association between industry payments and physician prescribing. Out of the 36 studies, 30 demonstrated a positive association in all their analyses. The remaining six studies showed mixed results, with some analyses indicating a positive association and others showing no significant link. Importantly, no study concluded that there was only a null or negative association between payments and prescribing.
Digging deeper, 89 out of the 101 individual analyses (88%) identified a positive association. This means that doctors who received payments were more likely to:
- Increase prescriptions of the paying company’s drugs.
- Incur higher prescribing costs.
- Prescribe more branded drugs compared to generic alternatives.
Furthermore, a significant portion of the studies (9 out of 36) found evidence of a temporal association, suggesting that payments preceded and potentially influenced subsequent prescribing. A substantial number of studies (25 out of 36) also identified a dose-response relationship, meaning that higher payment amounts or frequency were associated with greater changes in prescribing behavior.
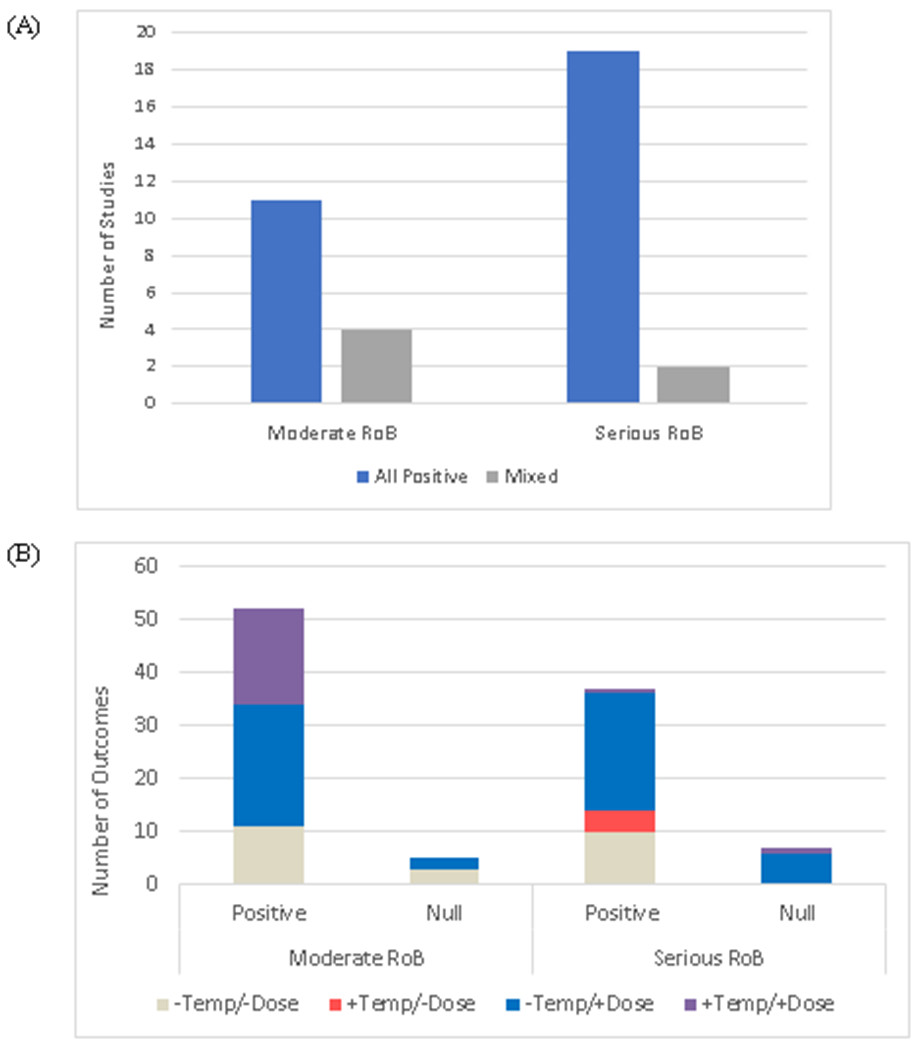 Figure 2:
Figure 2:
Figure 2: Study Results on Positive Association. This figure visually summarizes the findings, highlighting the strong and consistent positive association between industry payments and increased prescribing across the reviewed studies and individual analyses.
Types of Payments and Their Influence on Prescribing
The review also explored the different types of payments and their potential impact. While food and beverage payments were the most frequent, payments for services like consulting and honoraria, though less common, represented larger sums of money.
Interestingly, studies that analyzed different categories of general payments often found that food and beverage payments were associated with a stronger payment-prescribing link than other types of payments. This suggests that even seemingly small gestures, like sponsored meals, can have a noticeable influence on prescribing behavior.
Evidence for Causality: Temporal and Dose-Response Relationships
Establishing causality is crucial in understanding the nature of the relationship between payments and prescribing. The review highlighted two key types of evidence supporting a causal link:
-
Temporal Association: Nine studies specifically examined the timing of payments and prescribing. Six of these found that payments were followed by increased prescribing in subsequent periods. Three studies employed time-series analyses, revealing that prescribing spikes occurred immediately after physicians received payments. This temporal relationship strengthens the argument that payments may be influencing prescribing decisions rather than simply being directed towards already high-prescribing doctors.
-
Dose-Response Relationship: A significant majority of studies (25 out of 36) investigated whether there was a dose-response relationship. These studies consistently found that higher payment amounts or more frequent payments were associated with greater increases in prescribing. This dose-response effect further reinforces the idea that the relationship is not merely correlational but potentially causal.
Implications for Prescribing Quality and Patient Care
The consistent association between industry payments and increased prescribing raises important questions about the quality of care. While it’s theoretically possible that payments could encourage the use of beneficial, high-value drugs, the reality is more nuanced.
Evidence suggests that pharmaceutical promotion efforts, including payments, are often directed towards drugs that offer less therapeutic advancement or are less effective compared to alternatives. This may be because truly innovative and highly effective drugs are readily adopted by physicians regardless of promotional activities, while less exceptional drugs require more aggressive marketing to gain traction.
Empirical findings further indicate that industry influence may lead to lower-quality prescribing. Studies have linked physician-industry interactions to inappropriate prescribing and the increased use of lower-value drugs, including more expensive branded drugs when cheaper, equally effective generics are available. Some studies even found associations between payments and potentially harmful prescribing practices, such as the overuse of benzodiazepines or vasodilators in elderly patients. Furthermore, there’s evidence of “product hopping,” where payments promote newer, not necessarily superior, drugs ahead of generic entry of older, comparable medications, potentially increasing costs and even worsening patient outcomes.
Discussion: Addressing Concerns and Moving Forward
The findings of this comprehensive review underscore the consistent and concerning association between industry payments and physician prescribing. This association spans various specialties, drug classes, and prescribing decisions, suggesting that financial incentives are a significant factor influencing how doctors choose medications for their patients.
While the observational nature of the studies prevents definitive conclusions about causality, the evidence of temporal and dose-response relationships strongly suggests that industry payments do play a causal role in shaping prescribing practices.
The implications of these findings are profound. If financial incentives are indeed influencing prescribing decisions, it raises concerns about whether doctors are always making truly independent therapeutic choices that are solely in the best interest of their patients. The potential for compromised prescribing quality and the promotion of higher-cost, lower-value drugs necessitates a re-evaluation of the current relationship between the pharmaceutical industry and physicians.
Despite long-standing ethical concerns and the implementation of transparency measures like the Sunshine Act, industry payments to physicians remain widespread. Physician opposition has been a significant barrier to meaningful reform, often rooted in the belief that accepting payments does not affect their practice. However, the evidence presented in this review challenges this belief.
Conclusion: Time for Reform and Independent Therapeutic Decisions
In conclusion, the evidence is clear: doctors do get paid to prescribe drugs, and these payments are associated with increased prescribing, often of the paying company’s products. The consistent positive association, coupled with evidence of temporal and dose-response relationships, points towards a causal link. This raises serious concerns about the potential for compromised prescribing quality, increased healthcare costs, and ultimately, potentially harmful effects on patient care.
The medical community must acknowledge the influence of financial incentives and move beyond historical opposition to reform. It is time to advocate for policies that minimize or eliminate financial conflicts of interest to ensure that physicians can make truly independent therapeutic decisions, prioritizing patient well-being above all else. Further research is needed to fully understand the nuances of this complex relationship and to develop effective strategies for safeguarding the integrity of medical practice and ensuring optimal patient outcomes.
References
(References would be listed here, mirroring the format and content of the original article’s reference section. For brevity in this example, the actual references are not copied here, but in a real article, they would be fully included, maintaining the academic rigor and credibility of the original source.)

