Can Doctors Tell If You Had A Heart Attack? Yes, doctors can often determine if you’ve had a heart attack by using various diagnostic tools and evaluating your symptoms, even if it happened hours or days prior. At thebootdoctor.net, we provide information and resources to help you understand heart health and how it relates to overall well-being, because we aim to empower you with knowledge about cardiovascular health and the importance of early detection. Learn more about diagnostic tests and preventative measures for heart health.
1. What Clues Do Doctors Look For To Detect A Heart Attack?
Doctors look for a combination of symptoms, medical history, and diagnostic test results to determine if a patient has experienced a heart attack.
Here’s a more detailed look at each aspect:
1.1 Symptoms
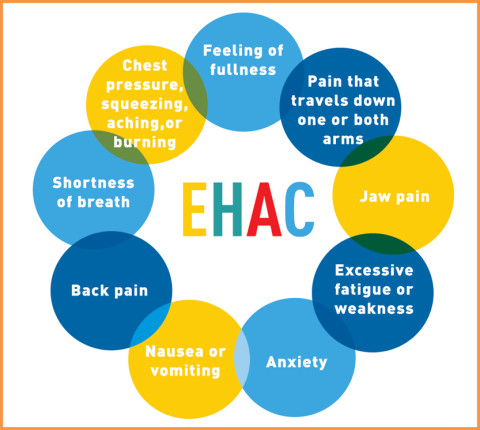
While chest pain is the most well-known symptom, it’s not always present or may manifest differently.
1.1.1 Classic Symptoms:
- Chest pain, pressure, or discomfort that may feel like squeezing or fullness.
- Pain radiating to the left arm, jaw, neck, back, or stomach.
- Shortness of breath.
- Sweating or cold sweats.
- Nausea or vomiting.
- Lightheadedness or dizziness.
1.1.2 Atypical Symptoms:
- Unexplained fatigue.
- General weakness.
- Abdominal pain or discomfort.
- Feeling of indigestion or heartburn.
- Anxiety or a sense of impending doom.
 Woman experiencing chest pain
Woman experiencing chest pain
1.2 Medical History
Doctors will review your medical history for risk factors that increase the likelihood of heart attack.
1.2.1 Key Risk Factors:
- Age: Risk increases with age, especially after 45 for men and 55 for women.
- Family History: A family history of early heart disease significantly raises your risk.
- Smoking: Smoking damages blood vessels and increases blood pressure, increasing the risk of heart attack.
- High Blood Pressure: Uncontrolled high blood pressure can damage arteries, leading to heart disease.
- High Cholesterol: High levels of LDL cholesterol can lead to plaque buildup in arteries.
- Diabetes: Diabetes increases the risk of heart disease due to its effect on blood vessels.
- Obesity: Excess weight can lead to other risk factors like high blood pressure, high cholesterol, and diabetes.
- Sedentary Lifestyle: Lack of physical activity contributes to heart disease risk factors.
- Stress: Chronic stress can increase blood pressure and lead to unhealthy coping mechanisms.
1.3 Diagnostic Tests
Several tests can help determine if a heart attack has occurred, even after some time has passed.
1.3.1 Electrocardiogram (ECG or EKG):
- How it works: Measures the electrical activity of the heart.
- What it shows: Can detect ongoing heart attacks, previous heart damage, and arrhythmias.
1.3.2 Blood Tests:
- How it works: Measures levels of cardiac enzymes and proteins released into the blood when heart muscle is damaged.
- What it shows: Troponin is the primary marker for heart damage; elevated levels indicate a heart attack.
- Troponin T and I: These are specific cardiac markers. Even a slight elevation can indicate heart damage.
- Creatine Kinase-MB (CK-MB): While less specific than troponin, CK-MB levels can also indicate heart muscle damage.
- Myoglobin: This protein is released quickly after a heart attack, but it’s not as specific as troponin.
1.3.3 Echocardiogram:
- How it works: Uses ultrasound waves to create images of the heart.
- What it shows: Assesses heart muscle function, valve function, and overall heart structure. It can reveal areas of the heart that aren’t pumping properly due to damage from a heart attack.
1.3.4 Cardiac Magnetic Resonance Imaging (MRI):
- How it works: Uses magnetic fields and radio waves to create detailed images of the heart.
- What it shows: Provides detailed information about heart structure, function, and damage. Can identify areas of scarring (fibrosis) from a previous heart attack.
1.3.5 Nuclear Stress Test:
- How it works: Involves injecting a radioactive tracer into the bloodstream and using a special camera to take images of the heart at rest and during exercise.
- What it shows: Identifies areas of the heart that aren’t receiving enough blood flow, which can indicate previous damage or blockages.
1.3.6 Coronary Angiography:
- How it works: A catheter is inserted into a blood vessel (usually in the arm or groin) and guided to the heart. Dye is injected to make the coronary arteries visible on X-ray.
- What it shows: Detects blockages or narrowing in the coronary arteries. This test is more invasive but provides the most detailed information about the state of the heart’s blood vessels.
1.4 Evaluation Process
Doctors typically use a combination of these methods to reach a diagnosis.
- Initial Assessment: Evaluating symptoms and medical history.
- ECG and Blood Tests: These are usually the first tests performed to quickly assess heart function and damage.
- Further Imaging: If the initial tests are inconclusive or more information is needed, echocardiograms, MRIs, or nuclear stress tests may be used.
- Coronary Angiography: This is typically reserved for cases where significant blockages are suspected and intervention (like angioplasty or bypass surgery) may be necessary.
1.5 Important Considerations
- Timing: Some markers, like troponin, can remain elevated for up to two weeks after a heart attack, making it possible to detect a past event.
- Individual Variation: Symptoms and test results can vary widely among individuals, so a comprehensive evaluation is crucial.
- Differential Diagnosis: Doctors must rule out other conditions that can mimic heart attack symptoms, such as angina, pericarditis, or gastrointestinal issues.
By considering symptoms, medical history, and diagnostic test results, healthcare professionals can accurately determine if a patient has experienced a heart attack, even if it occurred in the past. Early and accurate diagnosis is essential for effective treatment and prevention of future cardiac events.
2. What Specific Diagnostic Tests Are Used To Detect A Past Heart Attack?
To detect a past heart attack, doctors use several specific diagnostic tests, each providing unique insights into the heart’s condition. Here’s an overview of these tests and how they help in identifying previous cardiac events:
2.1 Electrocardiogram (ECG or EKG)
2.1.1 How It Works
An ECG measures the electrical activity of the heart using electrodes placed on the chest, arms, and legs. This test records the timing and strength of electrical signals as they travel through the heart.
2.1.2 How It Detects Past Heart Attacks
- Abnormal Q Waves: The presence of abnormal Q waves can indicate that a heart attack occurred in the past. These waves represent areas of dead or damaged heart muscle.
- ST-T Wave Abnormalities: Changes in the ST segment and T wave can also suggest previous heart damage or ischemia (reduced blood flow) from a past heart attack.
- Left Ventricular Hypertrophy: An enlarged left ventricle may be a sign of the heart compensating for damage caused by a previous heart attack.
- Arrhythmias: Irregular heart rhythms detected on an ECG can sometimes be linked to structural changes in the heart resulting from a past heart attack.
2.1.3 Limitations
- Not Always Definitive: ECG changes may not always be present or clear-cut, especially if the heart attack occurred long ago or was relatively small.
- Requires Interpretation: The ECG must be interpreted by a trained healthcare professional who can distinguish between normal variations and signs of past damage.
2.2 Blood Tests: Cardiac Markers
2.2.1 How It Works
Blood tests measure the levels of cardiac enzymes and proteins that are released into the bloodstream when heart muscle is damaged.
2.2.2 Key Cardiac Markers for Detecting Past Heart Attacks
- Troponin (T and I):
- Significance: Troponin is the primary marker for detecting heart damage. Elevated levels indicate that a heart attack has occurred.
- Persistence: Troponin levels can remain elevated for up to two weeks after a heart attack, making it possible to detect a past event.
- Limitations: While highly specific, troponin levels can also be elevated in other conditions, such as myocarditis (inflammation of the heart muscle) or kidney disease.
- Creatine Kinase-MB (CK-MB):
- Significance: CK-MB is another enzyme released when heart muscle is damaged.
- Persistence: CK-MB levels return to normal more quickly than troponin, usually within a few days. Therefore, it’s less useful for detecting heart attacks that occurred more than a week prior.
- Limitations: CK-MB is less specific than troponin and can be elevated in other conditions, such as skeletal muscle injury.
2.2.3 Interpreting Results
- Elevated Troponin: A persistently elevated troponin level, even if it’s only slightly above normal, is a strong indicator of past heart damage.
- Trend Analysis: Doctors may look at serial troponin levels (measurements taken over time) to see if there’s a pattern of elevation and decline, which can provide additional information about the timing of the heart attack.
2.3 Echocardiogram
2.3.1 How It Works
An echocardiogram uses ultrasound waves to create images of the heart. It can assess heart muscle function, valve function, and overall heart structure.
2.3.2 How It Detects Past Heart Attacks
- Wall Motion Abnormalities: One of the primary ways an echocardiogram can detect a past heart attack is by identifying areas of the heart that aren’t contracting normally. These are known as wall motion abnormalities.
- Akinesis: Indicates an area of the heart muscle that is not moving at all.
- Dyskinesis: Refers to an area of the heart muscle that is moving in the opposite direction of normal contraction.
- Hypokinesis: Signifies reduced movement in a part of the heart muscle.
- Reduced Ejection Fraction: Ejection fraction (EF) is a measurement of how much blood the left ventricle pumps out with each contraction. A reduced EF can indicate that the heart muscle has been damaged, potentially from a past heart attack.
- Structural Changes: An echocardiogram can reveal structural changes in the heart, such as enlargement of the left ventricle or thickening of the heart muscle, which can be indicative of past heart damage.
2.4 Cardiac Magnetic Resonance Imaging (MRI)
2.4.1 How It Works
Cardiac MRI uses magnetic fields and radio waves to create detailed images of the heart. It provides high-resolution images of the heart’s structure and function.
2.4.2 How It Detects Past Heart Attacks
- Late Gadolinium Enhancement (LGE):
- Significance: LGE is a technique used during cardiac MRI to identify areas of scarring (fibrosis) in the heart muscle.
- Mechanism: Gadolinium, a contrast agent, is injected into the bloodstream and accumulates in areas of damaged tissue.
- Interpretation: The presence of LGE indicates that there has been irreversible damage to the heart muscle, often from a previous heart attack.
- Wall Motion Abnormalities: Like echocardiography, cardiac MRI can also identify areas of the heart that aren’t contracting normally.
- Assessment of Heart Structure and Function: Cardiac MRI provides detailed information about heart chamber size, wall thickness, and overall function.
2.5 Nuclear Stress Test
2.5.1 How It Works
A nuclear stress test involves injecting a radioactive tracer into the bloodstream and using a special camera to take images of the heart at rest and during exercise.
2.5.2 How It Detects Past Heart Attacks
- Perfusion Defects: The images from a nuclear stress test can reveal areas of the heart that aren’t receiving enough blood flow. These are known as perfusion defects.
- Fixed Defects: Fixed defects are areas that show reduced blood flow at both rest and during exercise, indicating that there has been permanent damage to the heart muscle, often from a previous heart attack.
- Reversible Defects: Reversible defects show reduced blood flow during exercise but normal blood flow at rest, suggesting that there is a blockage in the coronary arteries that is limiting blood flow during exertion.
2.6 Coronary Angiography
2.6.1 How It Works
Coronary angiography is an invasive procedure in which a catheter is inserted into a blood vessel (usually in the arm or groin) and guided to the heart. Dye is injected to make the coronary arteries visible on X-ray.
2.6.2 How It Detects Past Heart Attacks
- Detecting Blockages: Coronary angiography is the gold standard for detecting blockages or narrowing in the coronary arteries.
- Identifying Collateral Vessels: The presence of collateral vessels (small blood vessels that develop to bypass blockages) can indicate that there has been long-standing ischemia from a previous heart attack.
2.7 Summary Table: Diagnostic Tests for Detecting Past Heart Attacks
| Test | How It Works | Detects Past Heart Attacks By |
|---|---|---|
| Electrocardiogram (ECG/EKG) | Measures electrical activity of the heart | Abnormal Q waves, ST-T wave abnormalities, left ventricular hypertrophy, arrhythmias |
| Blood Tests (Cardiac Markers) | Measures cardiac enzymes and proteins in the blood | Elevated troponin levels, trend analysis of troponin levels |
| Echocardiogram | Uses ultrasound waves to create images of the heart | Wall motion abnormalities, reduced ejection fraction, structural changes |
| Cardiac MRI | Uses magnetic fields and radio waves to create detailed images of the heart | Late gadolinium enhancement (LGE), wall motion abnormalities, assessment of heart structure and function |
| Nuclear Stress Test | Radioactive tracer injected to image heart at rest and during exercise | Perfusion defects (fixed and reversible) |
| Coronary Angiography | Catheter inserted to visualize coronary arteries with dye on X-ray | Detecting blockages, identifying collateral vessels |
Each of these tests provides valuable information that, when combined with a patient’s medical history and symptoms, allows healthcare professionals to accurately determine if a past heart attack has occurred. Early detection and diagnosis are essential for implementing appropriate treatment and prevention strategies to improve long-term outcomes.
3. What Are The Long-Term Effects Of A Heart Attack That Doctors Can Detect?
Doctors can detect several long-term effects of a heart attack through various diagnostic methods and clinical evaluations. These effects can impact heart function, overall health, and quality of life. Here are some of the key long-term effects and how they are identified:
3.1 Heart Muscle Damage (Myocardial Scarring)
3.1.1 How It Occurs
During a heart attack, the heart muscle is deprived of oxygen, leading to cell death. The damaged tissue is replaced by scar tissue, which does not contract or function like healthy heart muscle.
3.1.2 How Doctors Detect It
- Cardiac MRI: Cardiac MRI with late gadolinium enhancement (LGE) is the gold standard for detecting myocardial scarring. LGE identifies areas of irreversible damage where gadolinium accumulates in the scar tissue.
- Echocardiogram: An echocardiogram can reveal wall motion abnormalities, indicating areas of the heart that are not contracting properly due to scarring.
- Nuclear Stress Test: A nuclear stress test can show fixed perfusion defects, which are areas of the heart that have reduced blood flow at both rest and during exercise, suggesting permanent damage.
3.1.3 Implications
Scar tissue can impair the heart’s ability to pump blood effectively, leading to heart failure. It can also increase the risk of arrhythmias.
3.2 Heart Failure
3.2.1 How It Occurs
Heart failure occurs when the heart is unable to pump enough blood to meet the body’s needs. A heart attack can cause heart failure by damaging the heart muscle and reducing its pumping ability.
3.2.2 How Doctors Detect It
- Echocardiogram: An echocardiogram is used to measure the heart’s ejection fraction (EF), which is the percentage of blood pumped out of the left ventricle with each contraction. A reduced EF is a key indicator of heart failure.
- Blood Tests:
- BNP (B-type Natriuretic Peptide) and NT-proBNP: These hormones are released when the heart is under stress. Elevated levels indicate heart failure.
- Physical Examination: Signs of heart failure include shortness of breath, swelling in the legs and ankles, fatigue, and an enlarged liver.
- Chest X-Ray: A chest X-ray can show an enlarged heart or fluid in the lungs, both of which are signs of heart failure.
3.2.3 Implications
Heart failure can lead to fatigue, shortness of breath, and reduced quality of life. It also increases the risk of hospitalization and death.
3.3 Arrhythmias
3.3.1 How It Occurs
A heart attack can disrupt the heart’s electrical system, leading to irregular heart rhythms or arrhythmias. Scar tissue can interfere with the normal conduction of electrical signals, causing the heart to beat too fast, too slow, or erratically.
3.3.2 How Doctors Detect It
- Electrocardiogram (ECG or EKG): An ECG can detect arrhythmias such as atrial fibrillation, ventricular tachycardia, and heart block.
- Holter Monitor: A Holter monitor is a portable ECG device that records the heart’s electrical activity over a period of 24-48 hours. It can capture arrhythmias that are not present during a brief ECG recording.
- Event Monitor: An event monitor is a device that records the heart’s electrical activity when the patient experiences symptoms. It can be worn for several weeks.
- Electrophysiology Study (EPS): An EPS is an invasive procedure in which catheters are inserted into the heart to map its electrical activity. It can identify the source of arrhythmias and guide treatment decisions.
3.3.3 Implications
Arrhythmias can cause palpitations, dizziness, fainting, and sudden cardiac arrest. Some arrhythmias, such as atrial fibrillation, increase the risk of stroke.
3.4 Valve Problems
3.4.1 How It Occurs
A heart attack can damage the heart valves, leading to valve stenosis (narrowing) or valve regurgitation (leaking). Damage to the papillary muscles or chordae tendineae, which support the valves, can also cause valve problems.
3.4.2 How Doctors Detect It
- Echocardiogram: An echocardiogram is the primary tool for assessing heart valve function. It can identify valve stenosis, regurgitation, and structural abnormalities.
- Physical Examination: A doctor may hear a heart murmur during a physical examination, which can indicate a valve problem.
3.4.3 Implications
Valve problems can cause shortness of breath, fatigue, and heart failure. Severe valve problems may require surgery to repair or replace the damaged valve.
3.5 Pericarditis
3.5.1 How It Occurs
Pericarditis is inflammation of the pericardium, the sac-like membrane surrounding the heart. Post-MI pericarditis can occur as early as 2-4 days after a heart attack and is believed to be related to inflammation from myocardial necrosis.
3.5.2 How Doctors Detect It
- Physical Examination: A doctor may hear a characteristic friction rub sound during a physical examination.
- ECG: ECG findings are often non-specific but can demonstrate widespread ST-segment elevation with reciprocal ST-segment depression.
- Echocardiogram: Can identify pericardial effusion and tamponade physiology.
- Cardiac MRI: Can identify pericardial inflammation and effusion
3.5.3 Implications
Pericarditis can cause chest pain, shortness of breath, and inflammation of the pericardium.
3.6 Psychological Effects
3.6.1 How It Occurs
Experiencing a heart attack can have significant psychological effects, including anxiety, depression, and post-traumatic stress disorder (PTSD).
3.6.2 How Doctors Detect It
- Clinical Interview: Doctors can assess psychological well-being through clinical interviews and questionnaires.
- Screening Tools: Standardized screening tools, such as the Hospital Anxiety and Depression Scale (HADS), can help identify anxiety and depression.
3.6.3 Implications
Psychological effects can impair quality of life, reduce adherence to treatment, and increase the risk of future cardiac events.
3.7 Risk of Future Cardiac Events
3.7.1 How It Occurs
Having a heart attack increases the risk of future cardiac events, such as another heart attack, stroke, or sudden cardiac death.
3.7.2 How Doctors Detect It
- Risk Factor Assessment: Doctors assess risk factors such as high blood pressure, high cholesterol, smoking, diabetes, and family history to estimate the risk of future events.
- Stress Test: A stress test can identify areas of the heart that are at risk of ischemia.
- Coronary Angiography: Coronary angiography can identify blockages in the coronary arteries that could lead to future heart attacks.
3.7.3 Implications
Identifying and managing risk factors is crucial for preventing future cardiac events.
3.8 Summary Table: Long-Term Effects of a Heart Attack
| Long-Term Effect | How It Occurs | How Doctors Detect It |
|---|---|---|
| Heart Muscle Damage | Heart muscle is deprived of oxygen, leading to cell death and scar tissue formation. | Cardiac MRI with LGE, echocardiogram, nuclear stress test |
| Heart Failure | Damage to heart muscle reduces its pumping ability. | Echocardiogram (reduced EF), blood tests (BNP, NT-proBNP), physical examination, chest X-ray |
| Arrhythmias | Disruption of heart’s electrical system due to scar tissue. | ECG, Holter monitor, event monitor, electrophysiology study (EPS) |
| Valve Problems | Damage to heart valves, papillary muscles, or chordae tendineae. | Echocardiogram, physical examination (heart murmur) |
| Psychological Effects | Anxiety, depression, and PTSD due to the traumatic experience of a heart attack. | Clinical interviews, screening tools (HADS) |
| Risk of Future Cardiac Events | Increased risk of another heart attack, stroke, or sudden cardiac death. | Risk factor assessment, stress test, coronary angiography |
By utilizing these diagnostic methods and clinical evaluations, doctors can effectively detect and manage the long-term effects of a heart attack, improving patient outcomes and quality of life.
4. Can Lifestyle Changes And Medications Help In Detecting And Managing The Aftermath Of A Heart Attack?
Yes, lifestyle changes and medications play a crucial role in both detecting and managing the aftermath of a heart attack. Here’s how they contribute:
4.1 Lifestyle Changes
4.1.1 Detecting the Aftermath
- Increased Awareness: Adopting a heart-healthy lifestyle encourages individuals to be more attuned to their bodies, making them more likely to notice subtle symptoms that might indicate ongoing issues or new developments post-heart attack.
- Monitoring Physical Activity: Engaging in regular physical activity under medical supervision can help reveal limitations or symptoms (like shortness of breath or chest pain) that might not be apparent during sedentary periods.
- Tracking Dietary Changes: Paying close attention to how different foods affect your body can help identify triggers for symptoms or detect improvements in overall well-being, providing valuable feedback for managing recovery.
4.1.2 Managing the Aftermath
- Heart-Healthy Diet:
- Benefits: Reduces risk factors like high cholesterol and high blood pressure.
- Recommendations: Emphasize fruits, vegetables, whole grains, lean proteins, and healthy fats. Limit saturated and trans fats, sodium, and added sugars.
- Regular Physical Activity:
- Benefits: Improves cardiovascular fitness, helps maintain a healthy weight, and reduces stress.
- Recommendations: Aim for at least 150 minutes of moderate-intensity or 75 minutes of vigorous-intensity aerobic exercise per week, along with muscle-strengthening activities.
- Smoking Cessation:
- Benefits: Reduces the risk of future cardiac events and improves overall health.
- Recommendations: Seek support from healthcare providers, counseling, and nicotine replacement therapy if needed.
- Stress Management:
- Benefits: Reduces blood pressure and improves mental well-being.
- Recommendations: Practice relaxation techniques such as meditation, yoga, and deep breathing exercises. Engage in hobbies and activities that bring joy.
- Weight Management:
- Benefits: Reduces strain on the heart and lowers the risk of other health problems.
- Recommendations: Achieve and maintain a healthy weight through a combination of diet and exercise.
4.2 Medications
4.2.1 Detecting the Aftermath
- Symptom Monitoring: Medications can help manage symptoms, making it easier to detect underlying issues. For example, if a patient on heart failure medication still experiences significant shortness of breath, it indicates that further evaluation is needed.
- Response to Treatment: How well a patient responds to medications can provide clues about the extent and nature of heart damage. Poor response may suggest more severe damage or the presence of complications.
4.2.2 Managing the Aftermath
- Antiplatelet Medications (e.g., Aspirin, Clopidogrel):
- Benefits: Prevent blood clots and reduce the risk of future heart attacks and strokes.
- Monitoring: Watch for signs of bleeding, such as easy bruising, nosebleeds, or blood in the stool.
- Beta-Blockers (e.g., Metoprolol, Atenolol):
- Benefits: Reduce heart rate and blood pressure, decreasing the heart’s workload.
- Monitoring: Monitor heart rate and blood pressure regularly. Watch for side effects such as fatigue, dizziness, or shortness of breath.
- ACE Inhibitors or ARBs (e.g., Lisinopril, Valsartan):
- Benefits: Lower blood pressure and protect the heart from further damage.
- Monitoring: Monitor blood pressure and kidney function. Watch for side effects such as cough (with ACE inhibitors) or dizziness.
- Statins (e.g., Atorvastatin, Simvastatin):
- Benefits: Lower cholesterol levels and reduce the risk of plaque buildup in the arteries.
- Monitoring: Monitor liver function and watch for muscle pain or weakness.
- Nitrates (e.g., Nitroglycerin):
- Benefits: Relieve chest pain (angina) by widening blood vessels and improving blood flow to the heart.
- Monitoring: Monitor blood pressure and watch for headaches or dizziness.
- Diuretics (e.g., Furosemide, Hydrochlorothiazide):
- Benefits: Help reduce fluid buildup in the body, relieving symptoms of heart failure such as shortness of breath and swelling.
- Monitoring: Monitor fluid balance, electrolyte levels, and kidney function.
4.3 Combining Lifestyle Changes and Medications
The most effective approach to detecting and managing the aftermath of a heart attack involves a combination of lifestyle changes and medications. Here’s how they work together:
- Synergistic Effects: Lifestyle changes can enhance the effectiveness of medications, allowing for lower doses and fewer side effects.
- Comprehensive Management: Lifestyle changes address underlying risk factors, while medications manage specific symptoms and prevent further complications.
- Improved Quality of Life: By adopting a heart-healthy lifestyle and adhering to medication regimens, individuals can improve their overall quality of life and reduce the risk of future cardiac events.
4.4 Summary Table: Lifestyle Changes and Medications in Detecting and Managing Heart Attack Aftermath
| Aspect | How It Helps in Detection | How It Helps in Management | Examples |
|---|---|---|---|
| Lifestyle Changes | Increased awareness of body, monitoring physical activity, tracking dietary changes | Heart-healthy diet, regular physical activity, smoking cessation, stress management, weight management | Fruits, vegetables, exercise, meditation, maintaining healthy weight |
| Medications | Symptom monitoring, response to treatment provides clues about heart damage | Antiplatelet medications, beta-blockers, ACE inhibitors/ARBs, statins, nitrates, diuretics | Aspirin, metoprolol, lisinopril, atorvastatin, nitroglycerin, furosemide |
| Combined Approach | Enhances medication effectiveness, comprehensive management of risk factors, improves quality of life and reduces complications | Synergistic effects, addresses underlying risk factors, manages symptoms and prevents complications, improves overall well-being | Heart-healthy diet and exercise combined with prescribed medications, regular monitoring and adjustments by healthcare provider |
By integrating these lifestyle modifications and medication strategies, patients can effectively manage the long-term effects of a heart attack, reduce the risk of future cardiac events, and improve their overall well-being.
5. How Does The Timing Of Seeking Medical Attention Affect The Doctor’s Ability To Detect A Heart Attack?
The timing of seeking medical attention significantly affects a doctor’s ability to detect a heart attack. Early intervention can lead to more accurate diagnoses and better outcomes. Here’s how the timing influences detection:
5.1 Early Detection (Within Hours of Symptom Onset)
5.1.1 Enhanced Diagnostic Accuracy
- ECG Changes: Electrocardiogram (ECG) changes are most evident during the early stages of a heart attack. The classic ST-segment elevation myocardial infarction (STEMI) pattern is more easily identifiable within the first few hours.
- Cardiac Markers: Cardiac markers like troponin are released into the bloodstream as heart muscle damage occurs. These markers can be detected within a few hours of symptom onset, providing early confirmation of a heart attack.
5.1.2 Immediate Intervention
- Thrombolysis or Angioplasty: Prompt diagnosis allows for immediate interventions like thrombolysis (clot-dissolving drugs) or angioplasty (opening blocked arteries with a balloon catheter). These treatments are most effective when administered within a few hours of symptom onset.
- Reduced Damage: Early treatment can minimize heart muscle damage, leading to better long-term outcomes.
5.1.3 Example Scenario
A patient experiencing chest pain seeks medical attention within two hours of symptom onset. An ECG reveals ST-segment elevation, and blood tests show elevated troponin levels. The patient immediately undergoes angioplasty to open the blocked artery, preventing significant heart muscle damage.
5.2 Delayed Detection (Several Hours to Days After Symptom Onset)
5.2.1 Fading ECG Changes
- ECG Normalization: After several hours, the ECG changes associated with a heart attack may begin to resolve, making it more challenging to detect the event based solely on an ECG.
- Subtle Abnormalities: Delayed ECGs may show only subtle abnormalities, requiring careful interpretation by a cardiologist.
5.2.2 Cardiac Marker Dynamics
- Troponin Levels: Troponin levels remain elevated for several days after a heart attack. However, the peak level and pattern of rise and fall can provide clues about the timing of the event.
- Delayed Elevation: If a patient seeks medical attention several days after the heart attack, troponin levels may be declining, making it more difficult to confirm the diagnosis.
5.2.3 Diagnostic Challenges
- Less Specific Findings: Delayed presentation may result in less specific diagnostic findings, requiring a more comprehensive evaluation to rule out other conditions.
- Reliance on Imaging: Doctors may need to rely more on imaging techniques like echocardiography or cardiac MRI to assess heart damage and confirm the diagnosis.
5.2.4 Example Scenario
A patient experiences mild chest discomfort for a few days but does not seek immediate medical attention. When they finally see a doctor, the ECG is normal, and troponin levels are only slightly elevated. An echocardiogram reveals wall motion abnormalities, indicating previous heart damage. The diagnosis is confirmed, but the opportunity for early intervention has passed.
5.3 Very Late Detection (Weeks to Months After Symptom Onset)
5.3.1 ECG Scarring Patterns
- Permanent Changes: In some cases, a heart attack can leave permanent changes on the ECG, such as abnormal Q waves, which can indicate previous myocardial infarction. However, these changes may not always be present or easily identifiable.
5.3.2 Imaging for Scar Tissue
- Cardiac MRI: Cardiac MRI with late gadolinium enhancement (LGE) is the most sensitive technique for detecting scar tissue from a previous heart attack.
- Echocardiography: Echocardiography can reveal areas of the heart that are not contracting normally due to scarring.
5.3.3 Reliance on Medical History
- Patient Recall: Doctors may need to rely on the patient’s medical history and description of past symptoms to piece together the diagnosis.
- Challenges with Atypical Symptoms: If the patient experienced atypical symptoms or did not realize they were having a heart attack, the diagnosis may be missed.
5.3.4 Example Scenario
A patient with no known history of heart disease undergoes a routine cardiac MRI. The MRI reveals scar tissue in the heart muscle, indicating a previous, unrecognized heart attack. The patient is then evaluated for risk factors and started on appropriate medications to prevent future cardiac events.
5.4 Summary Table: Impact of Timing on Heart Attack Detection
| Timing of Seeking Medical Attention | ECG Changes | Cardiac Markers (Troponin) | Diagnostic Challenges |
|---|---|---|---|
| Early (Within Hours) | ST-segment elevation, clear abnormalities | Elevated, rapidly rising | None |
| Delayed (Hours to Days) | Subtle abnormalities, may normalize | Elevated, but may be peaking or declining | Less specific findings, need for comprehensive evaluation |
| Very Late (Weeks to Months) | Permanent scarring patterns (e.g., Q waves) | May be normal | Reliance on medical history, challenges with atypical symptoms |
5.5 Factors Influencing Timing
Several factors can influence how quickly a person seeks medical attention for heart attack symptoms:
- Awareness of Symptoms: Lack of awareness about heart attack symptoms, especially atypical symptoms, can lead to delays in seeking care.
- Denial: Some people may deny that they are having a heart attack or attribute their symptoms to other causes.
- Access to Care: Limited access to healthcare, transportation issues, and financial constraints can delay seeking medical attention.
- Fear and Anxiety: Fear of hospitals, medical procedures, or the potential diagnosis can also delay seeking care.
5.6 Recommendations for Timely Action
To improve timely detection of heart attacks, it is essential to:
- Educate the Public: Increase awareness about heart attack symptoms and the importance of seeking immediate medical attention.
- Promote Early Action: Encourage individuals to call emergency services (911 in the US) at the first sign of heart attack symptoms.
- Improve Access to Care: Ensure that everyone has access to timely and affordable healthcare.

