Alcoholic liver disease is a serious condition, and you may wonder, Can Doctors Tell If Liver Damage Is Caused By Alcohol? At thebootdoctor.net, we can tell you that the answer is generally yes, as doctors use various tests and evaluations to determine the cause and extent of liver damage. Early detection is key to managing the condition and preventing further complications. Understanding the diagnostic process can help you take proactive steps toward your liver health.
1. What Is Alcoholic Liver Disease?
Alcoholic liver disease (ALD) is liver damage caused by excessive alcohol consumption. The liver processes alcohol, and heavy drinking can overwhelm this process, leading to liver inflammation and damage. Over time, this can result in serious conditions such as cirrhosis.
1.1. The Liver’s Role in Your Body
The liver plays a vital role in maintaining overall health. According to the National Institutes of Health (NIH), the liver performs several essential functions:
- Detoxifying blood by removing harmful substances.
- Producing bile, which aids in digestion and absorption of fats.
- Storing glucose for energy.
- Manufacturing proteins for blood clotting and other important processes.
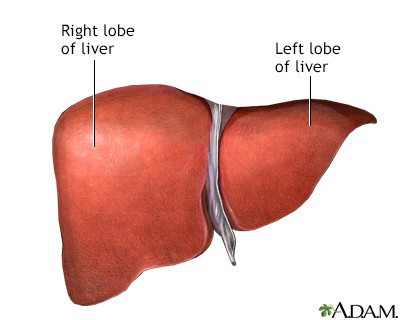 Liver anatomy
Liver anatomy
Alt: A detailed anatomical illustration of the liver, highlighting its major lobes, blood vessels, and surrounding structures within the abdominal cavity.
1.2. How Alcohol Affects the Liver
When you drink alcohol, the liver metabolizes it into toxic byproducts like acetaldehyde. According to a study from the National Institute on Alcohol Abuse and Alcoholism (NIAAA) in July 2023, acetaldehyde can damage liver cells, leading to inflammation and cell death. Prolonged heavy drinking can result in:
- Fatty Liver (Steatosis): Accumulation of fat in the liver cells.
- Alcoholic Hepatitis: Inflammation and damage to liver cells.
- Cirrhosis: Scarring of the liver, which impairs its function.
2. How Do Doctors Diagnose Alcoholic Liver Damage?
Doctors use a combination of medical history, physical exams, and diagnostic tests to determine if liver damage is caused by alcohol.
2.1. Medical History and Alcohol Consumption
Your doctor will start by asking detailed questions about your medical history and alcohol consumption. This includes:
- How much alcohol you drink on average.
- How often you drink alcohol.
- The duration of your heavy drinking.
- Any history of liver disease or other medical conditions.
2.2. Physical Examination
During a physical exam, your doctor will look for signs of liver damage, such as:
- An enlarged liver (hepatomegaly) or spleen (splenomegaly).
- Yellowing of the skin and eyes (jaundice).
- Fluid buildup in the abdomen (ascites) or legs (edema).
- Small, red spider-like blood vessels on the skin (spider angiomas).
- Redness of the palms (palmar erythema).
2.3. Liver Function Tests (LFTs)
Liver function tests are blood tests that measure the levels of various enzymes and proteins produced by the liver. Abnormal levels can indicate liver damage. Key LFTs include:
- Alanine Aminotransferase (ALT): An enzyme released into the blood when the liver is damaged.
- Aspartate Aminotransferase (AST): Another enzyme that indicates liver damage.
- Alkaline Phosphatase (ALP): An enzyme that can indicate bile duct obstruction or liver inflammation.
- Bilirubin: A yellow pigment produced during the breakdown of red blood cells; elevated levels cause jaundice.
- Albumin: A protein produced by the liver; low levels can indicate liver damage.
- Prothrombin Time (PT): Measures how long it takes for blood to clot; prolonged PT can indicate impaired liver function.
2.4. Blood Tests
In addition to LFTs, other blood tests can help determine if alcohol is the cause of liver damage. These include:
- Gamma-Glutamyl Transferase (GGT): An enzyme that is highly sensitive to alcohol-induced liver damage.
- Carbohydrate-Deficient Transferrin (CDT): A marker that can help identify chronic heavy alcohol consumption.
- Complete Blood Count (CBC): To check for anemia or other blood abnormalities that can be associated with liver disease.
2.5. Imaging Studies
Imaging studies provide detailed pictures of the liver and can help identify abnormalities. Common imaging techniques include:
- Ultrasound: A non-invasive test that uses sound waves to create images of the liver.
- CT Scan: A more detailed imaging technique that uses X-rays to create cross-sectional images of the liver.
- MRI: Uses magnetic fields and radio waves to create detailed images of the liver.
- FibroScan: A non-invasive test that measures liver stiffness, which can indicate fibrosis or cirrhosis.
2.6. Liver Biopsy
A liver biopsy is the most definitive way to diagnose alcoholic liver disease. It involves taking a small sample of liver tissue for examination under a microscope. According to the American Liver Foundation, a liver biopsy can:
- Confirm the diagnosis of alcoholic liver disease.
- Determine the extent of liver damage.
- Rule out other causes of liver disease.
3. Differentiating Alcoholic Liver Disease from Other Liver Conditions
It’s important to differentiate alcoholic liver disease from other liver conditions, as the treatment and management strategies may differ.
3.1. Non-Alcoholic Fatty Liver Disease (NAFLD)
Non-alcoholic fatty liver disease (NAFLD) is a condition in which fat accumulates in the liver of people who don’t drink heavily. According to the Mayo Clinic, NAFLD is often associated with obesity, diabetes, and high cholesterol. To differentiate NAFLD from ALD, doctors consider:
- Alcohol consumption history.
- Presence of metabolic risk factors (e.g., obesity, diabetes).
- Liver biopsy findings.
3.2. Viral Hepatitis
Viral hepatitis (such as hepatitis B and hepatitis C) can also cause liver damage. Blood tests can detect the presence of hepatitis viruses. Unlike ALD, viral hepatitis has specific antiviral treatments.
3.3. Autoimmune Liver Diseases
Autoimmune liver diseases, such as autoimmune hepatitis and primary biliary cholangitis, occur when the immune system attacks the liver. Blood tests to detect specific antibodies can help diagnose these conditions.
3.4. Genetic Liver Diseases
Certain genetic conditions, such as hemochromatosis and Wilson’s disease, can also cause liver damage. Genetic testing and specific blood tests can help diagnose these conditions.
4. Symptoms of Alcoholic Liver Disease
The symptoms of alcoholic liver disease can vary depending on the stage of the disease. Some people may have no symptoms in the early stages, while others may experience severe symptoms.
4.1. Early Symptoms
Early symptoms of alcoholic liver disease may include:
- Fatigue
- Loss of appetite
- Nausea
- Abdominal discomfort
- Weight loss
4.2. Advanced Symptoms
As liver function worsens, more severe symptoms may develop, including:
- Jaundice (yellowing of the skin and eyes)
- Ascites (fluid buildup in the abdomen)
- Edema (swelling in the legs and ankles)
- Hepatic encephalopathy (confusion, disorientation, or coma)
- Variceal bleeding (bleeding from enlarged veins in the esophagus or stomach)
- Easy bruising and bleeding
5. Treatment Options for Alcoholic Liver Disease
The primary goal of treatment for alcoholic liver disease is to stop further liver damage and manage symptoms.
5.1. Alcohol Abstinence
Abstaining from alcohol is the most important step in treating alcoholic liver disease. According to the National Institute on Alcohol Abuse and Alcoholism (NIAAA), quitting alcohol can improve liver function and prevent further damage.
5.2. Nutritional Support
Many people with alcoholic liver disease are malnourished. A healthy diet can help improve liver function and overall health. Nutritional support may include:
- A high-calorie diet to promote weight gain.
- Vitamin and mineral supplements to correct deficiencies.
- Limiting sodium intake to reduce fluid retention.
5.3. Medications
Several medications may be used to treat alcoholic liver disease and manage its complications:
- Corticosteroids: To reduce liver inflammation in severe cases of alcoholic hepatitis.
- Pentoxifylline: Another medication that may reduce liver inflammation.
- Diuretics: To reduce fluid buildup in the abdomen and legs.
- Lactulose: To reduce ammonia levels in the blood and prevent hepatic encephalopathy.
- Antibiotics: To treat infections.
5.4. Liver Transplant
In severe cases of cirrhosis, a liver transplant may be the only option. Liver transplantation involves replacing the damaged liver with a healthy liver from a deceased or living donor. To be eligible for a liver transplant, individuals must meet certain criteria, including:
- Abstaining from alcohol for at least six months.
- Having severe liver damage that is unlikely to improve with other treatments.
- Being otherwise healthy enough to undergo surgery.
6. Lifestyle Changes to Support Liver Health
In addition to medical treatment, certain lifestyle changes can support liver health.
6.1. Healthy Diet
A healthy diet is essential for liver health. Focus on:
- Eating plenty of fruits and vegetables.
- Choosing lean protein sources.
- Limiting processed foods, sugary drinks, and saturated fats.
6.2. Regular Exercise
Regular exercise can help improve liver function and overall health. Aim for at least 150 minutes of moderate-intensity exercise per week.
6.3. Avoid Toxins
Minimize exposure to toxins that can damage the liver, such as:
- Certain medications.
- Environmental pollutants.
- Chemicals in cleaning products.
6.4. Vaccinations
Get vaccinated against hepatitis A and hepatitis B to protect your liver from viral infections.
7. Complications of Alcoholic Liver Disease
If left untreated, alcoholic liver disease can lead to several serious complications.
7.1. Cirrhosis
Cirrhosis is a late-stage complication of alcoholic liver disease characterized by scarring of the liver. Cirrhosis can lead to:
- Portal hypertension (increased pressure in the blood vessels of the liver).
- Variceal bleeding (bleeding from enlarged veins in the esophagus or stomach).
- Ascites (fluid buildup in the abdomen).
- Hepatic encephalopathy (confusion, disorientation, or coma).
- Liver cancer.
7.2. Liver Cancer
Alcoholic liver disease increases the risk of liver cancer, also known as hepatocellular carcinoma. Regular screening for liver cancer is recommended for people with cirrhosis.
7.3. Hepatic Encephalopathy
Hepatic encephalopathy is a condition in which the brain is affected by toxins that the liver is unable to remove. Symptoms can range from mild confusion to coma.
7.4. Ascites and Spontaneous Bacterial Peritonitis
Ascites is the accumulation of fluid in the abdomen, which can become infected, leading to spontaneous bacterial peritonitis (SBP).
7.5. Kidney Failure
Severe liver disease can lead to kidney failure, also known as hepatorenal syndrome.
8. Seeking Professional Help
If you are concerned about your alcohol consumption or think you may have liver damage, it’s important to seek professional help.
8.1. When to See a Doctor
Contact your doctor if you experience any of the following symptoms:
- Fatigue
- Loss of appetite
- Nausea
- Abdominal pain
- Jaundice
- Swelling in the legs or abdomen
- Confusion or disorientation
8.2. Finding a Liver Specialist
A hepatologist is a doctor who specializes in liver diseases. They can provide expert care and guidance for managing alcoholic liver disease. You can find a hepatologist through referrals from your primary care doctor or by searching online directories.
8.3. Support Groups and Resources
Joining a support group can provide emotional support and practical advice for people with alcoholic liver disease and their families. Resources include:
- Alcoholics Anonymous (AA)
- American Liver Foundation
- National Institute on Alcohol Abuse and Alcoholism (NIAAA)
9. Prevention Strategies
Preventing alcoholic liver disease involves making informed choices about alcohol consumption.
9.1. Moderate Alcohol Consumption
If you choose to drink alcohol, do so in moderation. According to the Dietary Guidelines for Americans, moderate alcohol consumption is defined as:
- Up to one drink per day for women.
- Up to two drinks per day for men.
9.2. Avoiding Binge Drinking
Binge drinking (consuming a large amount of alcohol in a short period) can significantly increase the risk of liver damage.
9.3. Regular Check-Ups
Regular check-ups with your doctor can help detect liver problems early.
10. Latest Research and Developments
The field of liver disease is constantly evolving, with new research and developments emerging.
10.1. New Treatments for Alcoholic Hepatitis
Researchers are exploring new treatments for alcoholic hepatitis, including medications that target liver inflammation and promote liver regeneration.
10.2. Advances in Liver Transplantation
Advances in liver transplantation techniques and immunosuppressive medications have improved outcomes for people with severe liver disease.
10.3. Non-Invasive Diagnostic Tools
Non-invasive diagnostic tools, such as FibroScan, are becoming more widely used to assess liver damage without the need for a liver biopsy.
FAQ: Understanding Alcoholic Liver Disease
1. Can liver damage from alcohol be reversed?
Yes, in the early stages, such as fatty liver, the liver can heal if you stop drinking alcohol. However, cirrhosis is often irreversible.
2. How much alcohol is too much for the liver?
It varies, but generally, more than 2-3 drinks per day regularly can lead to liver damage.
3. What are the first signs of liver damage from alcohol?
Early signs include fatigue, loss of appetite, and abdominal discomfort.
4. How long does it take to develop alcoholic liver disease?
It usually takes years of heavy drinking, but the exact timeline varies.
5. Can women develop alcoholic liver disease faster than men?
Yes, women are generally more susceptible to alcohol-related liver damage.
6. What tests are used to diagnose alcoholic liver disease?
Liver function tests, blood tests, imaging studies, and liver biopsy.
7. Is there a cure for alcoholic liver disease?
There is no cure, but abstinence from alcohol and medical treatment can manage the condition.
8. Can I still drink alcohol if I have fatty liver?
No, it’s best to abstain from alcohol to allow your liver to heal.
9. What is the role of diet in managing alcoholic liver disease?
A healthy diet supports liver function and overall health.
10. Where can I find support for alcoholic liver disease?
Support groups, medical professionals, and organizations like the American Liver Foundation.
Understanding how doctors diagnose alcoholic liver disease can empower you to take proactive steps toward your liver health. If you are concerned about your alcohol consumption or have symptoms of liver disease, consult with a healthcare professional for evaluation and guidance. Visit thebootdoctor.net for more information on maintaining your health and well-being.
Address: 6565 Fannin St, Houston, TX 77030, United States. Phone: +1 (713) 791-1414. Website: thebootdoctor.net.
 CT scan of the upper abdomen showing a fatty liver (steatosis of the liver). Note the liver enlargement and dark color compared with the spleen (gray body in lower right).
CT scan of the upper abdomen showing a fatty liver (steatosis of the liver). Note the liver enlargement and dark color compared with the spleen (gray body in lower right).
Alt: A CT scan illustrating steatosis of the liver, with liver enlargement and a darker color contrast compared to the spleen.
The information provided on thebootdoctor.net is intended for general knowledge and informational purposes only, and does not constitute medical advice. It is essential to consult with a qualified healthcare professional for any health concerns or before making any decisions related to your health or treatment. At thebootdoctor.net, we are committed to providing reliable and accessible health information to support your well-being.


