Can A Nurse Practitioner Call Themselves Doctor? Yes, a nurse practitioner with a Doctor of Nursing Practice (DNP) can use the title “Doctor,” but it’s crucial to ensure clarity in a clinical setting to avoid patient confusion; we at thebootdoctor.net aim to shed light on this complex topic, emphasizing transparency and ethical practice. This detailed guide clarifies the nuances of scope of practice, proper titles, and the importance of clear communication in healthcare, with resources and expert insights available on thebootdoctor.net. You’ll also learn about patient safety, clinical setting, and healthcare professionals.
1. What Is A Nurse Practitioner (NP)?
Yes, a Nurse Practitioner (NP) is an advanced practice registered nurse (APRN) who has completed a master’s or doctoral degree program and is certified to provide a wide range of healthcare services. These healthcare services often include diagnosing and treating illnesses, prescribing medications, and ordering and interpreting diagnostic tests. Nurse practitioners play a vital role in expanding access to quality healthcare, particularly in underserved areas, and are an essential part of the healthcare system.
Nurse practitioners (NPs) hold a pivotal role in the healthcare landscape, functioning as advanced practice registered nurses (APRNs). To become an NP, one must complete a master’s or doctoral degree program, followed by certification in a specialized area. This rigorous training equips NPs with the expertise to deliver a broad spectrum of healthcare services, contributing significantly to the well-being of patients across various settings.
1.1 The Role Of Nurse Practitioners In Healthcare
Nurse practitioners serve as primary and specialty care providers in various settings, including hospitals, clinics, private practices, and community health centers. They work both independently and in collaboration with physicians to deliver comprehensive care to patients of all ages. Their responsibilities often include:
- Performing physical exams
- Ordering and interpreting diagnostic tests
- Diagnosing and treating acute and chronic illnesses
- Prescribing medications
- Providing patient education and counseling
- Managing overall patient care
1.2 Education And Training Of Nurse Practitioners
The journey to becoming a nurse practitioner involves a substantial commitment to education and training. Individuals typically begin by earning a Bachelor of Science in Nursing (BSN) degree, followed by gaining experience as a registered nurse (RN). To advance to the role of an NP, they must complete a Master of Science in Nursing (MSN) or a Doctor of Nursing Practice (DNP) program.
These advanced degree programs provide NPs with specialized knowledge and skills in areas such as:
- Advanced pathophysiology
- Advanced pharmacology
- Advanced health assessment
- Diagnosis and treatment of medical conditions
- Healthcare management and leadership
In addition to coursework, NP students complete clinical rotations under the supervision of experienced healthcare professionals, gaining hands-on experience in their chosen specialty. Upon graduation, they must pass a national certification exam to become licensed and practice as a nurse practitioner.
1.3 Scope Of Practice For Nurse Practitioners
The scope of practice for nurse practitioners varies by state, but generally includes the ability to:
- Evaluate and manage patient conditions
- Order and interpret diagnostic tests
- Prescribe medications
- Perform certain medical procedures
In some states, NPs have full practice authority, allowing them to practice independently without physician oversight. In other states, NPs must practice under the supervision or collaboration of a physician. Despite these variations, nurse practitioners consistently demonstrate their ability to provide high-quality, cost-effective care to patients across diverse populations.
2. What Is A Doctor Of Nursing Practice (DNP)?
A Doctor of Nursing Practice (DNP) is a terminal degree in nursing, representing the highest level of education for nurse practitioners and other advanced practice registered nurses (APRNs), such as nurse midwives, clinical nurse specialists, and nurse anesthetists. DNP programs focus on equipping nurses with the knowledge and skills to improve healthcare outcomes through evidence-based practice, quality improvement, and systems leadership. It is designed to prepare nurses to be leaders in healthcare and to improve patient outcomes through the application of research and evidence-based practice.
2.1 DNP Curriculum And Focus
DNP programs typically cover a wide range of topics, including:
- Evidence-based practice
- Quality improvement
- Healthcare policy
- Leadership and management
- Informatics
- Population health
The curriculum is designed to equip graduates with the knowledge and skills to translate research findings into practice, lead healthcare teams, and advocate for policies that improve patient care.
2.2 Goals Of A DNP Program
The primary goals of a DNP program include:
- Preparing nurses to lead healthcare teams and organizations
- Equipping nurses with the skills to translate research into practice
- Improving healthcare outcomes through evidence-based practice
- Advocating for policies that promote patient safety and quality care
- Advancing the nursing profession through scholarship and leadership
2.3 DNP Vs. Phd In Nursing
While both DNP and PhD degrees represent the highest level of education in nursing, they serve distinct purposes. The DNP is a practice-focused degree, designed to prepare nurses for leadership roles in clinical settings. In contrast, the PhD is a research-focused degree, designed to prepare nurses for careers in academia and research.
| Feature | DNP (Doctor of Nursing Practice) | PhD in Nursing |
|---|---|---|
| Focus | Clinical practice and leadership | Research and academia |
| Goal | Improve healthcare outcomes through practice | Advance nursing knowledge through research |
| Curriculum | Evidence-based practice, quality improvement | Research methods, statistics, theory development |
| Career Path | Advanced practice roles, healthcare leadership | Professor, researcher |
| Emphasis | Applying research to clinical practice | Conducting original research |
| Terminal Degree | Yes, for clinical practice | Yes, for research and academia |
While DNP graduates may engage in some research activities, their primary focus is on applying existing knowledge to improve patient care. PhD graduates, on the other hand, are primarily focused on generating new knowledge through original research.
3. Can A DNP Call Themselves “Doctor”?
Yes, a DNP can use the title “Doctor,” as they have earned a doctoral degree. However, it is essential to ensure that they clearly communicate their credentials and role to patients to avoid confusion and maintain transparency. Transparency and clarity are key when a DNP uses the title “Doctor,” especially in clinical settings; it ensures that patients understand the qualifications and role of their healthcare provider, promoting trust and informed decision-making.
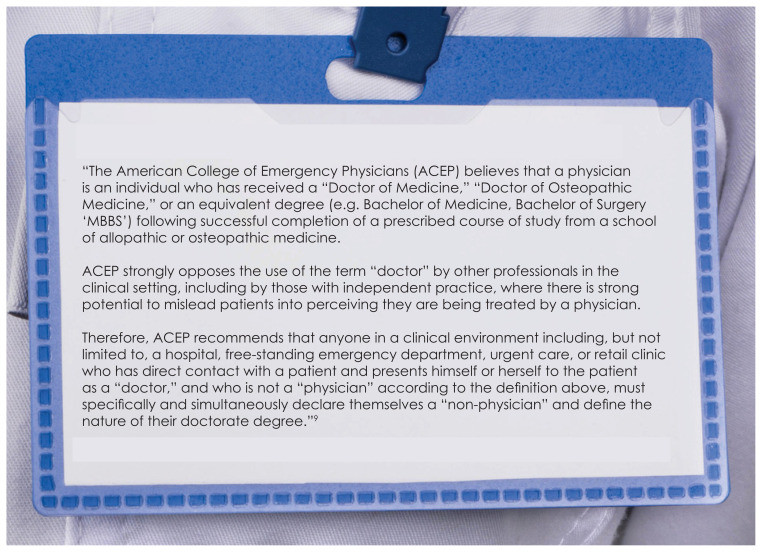
3.1 Ethical Considerations
The use of the title “Doctor” by DNPs raises ethical considerations, particularly in clinical settings where patients may assume that anyone using the title is a medical doctor (MD or DO). To avoid misleading patients, DNPs should always clearly identify themselves as nurse practitioners and specify their credentials. This can be done through verbal communication, written materials, and signage.
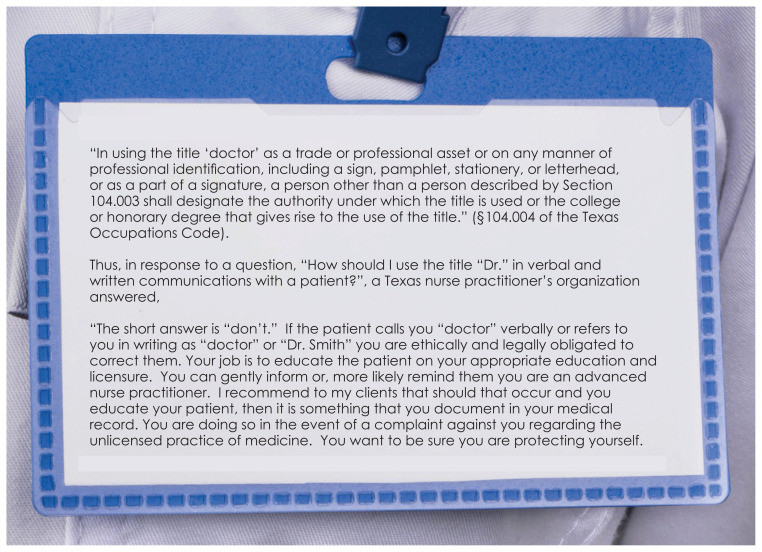
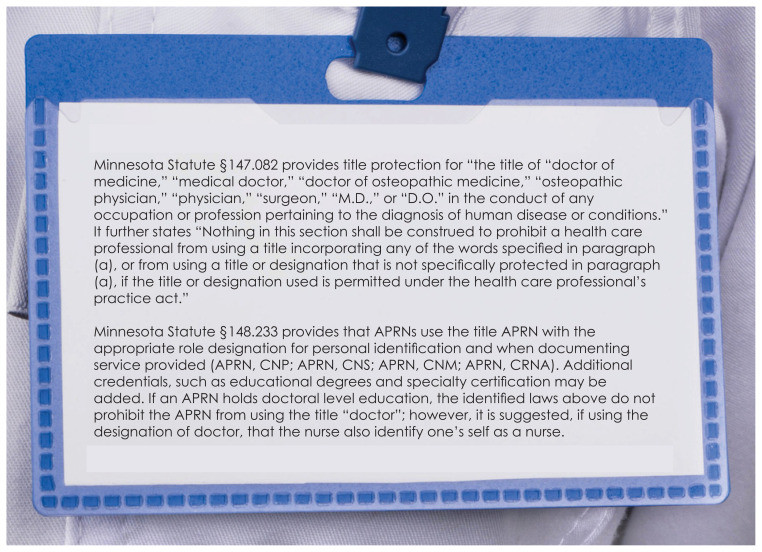
3.2 Legal Regulations
Some states have specific regulations regarding the use of the title “Doctor” by non-physicians. These laws are designed to protect patients from deception and ensure that they understand the qualifications of their healthcare providers. DNPs should be aware of the laws in their state and comply with all applicable regulations.
3.3 Guidelines From Nursing Organizations
Nursing organizations such as the American Association of Nurse Practitioners (AANP) and the National Council of State Boards of Nursing (NCSBN) have issued guidelines on the use of the title “Doctor” by DNPs. These guidelines emphasize the importance of transparency and clear communication with patients. They also recommend that DNPs use their credentials (e.g., DNP, APRN) in conjunction with the title “Doctor” to avoid confusion.
4. The Importance Of Transparency In Healthcare
Transparency in healthcare is essential for building trust between patients and providers, promoting informed decision-making, and ensuring patient safety. When healthcare providers are transparent about their qualifications, roles, and treatment plans, patients are better able to participate in their care and make informed choices about their health.
4.1 Building Patient Trust
Transparency is a cornerstone of the patient-provider relationship. When healthcare providers are open and honest about their qualifications, experience, and treatment approaches, patients are more likely to trust them. This trust is essential for effective communication, shared decision-making, and adherence to treatment plans.
4.2 Promoting Informed Decision-Making
Informed decision-making is a fundamental right of patients. To make informed decisions about their health, patients need access to accurate and understandable information about their medical conditions, treatment options, and the qualifications of their healthcare providers. Transparency ensures that patients have the information they need to make choices that align with their values and preferences.
4.3 Ensuring Patient Safety
Transparency also plays a crucial role in ensuring patient safety. When healthcare providers are transparent about potential risks and complications associated with treatments, patients can make informed decisions about whether to proceed. Additionally, transparency about errors and adverse events can help prevent future harm and improve the quality of care.
5. How To Properly Identify A DNP In A Clinical Setting
To avoid confusion and maintain transparency, DNPs should always clearly identify themselves in clinical settings. This can be achieved through various methods, including:
5.1 Verbal Communication
When introducing themselves to patients, DNPs should use clear and concise language to explain their role and qualifications. For example, they might say, “Hello, my name is Dr. [Name], and I am a Doctor of Nursing Practice and a board-certified nurse practitioner.” This statement clearly conveys that the provider is a nurse practitioner with a doctoral degree in nursing.
5.2 Written Materials
Written materials such as business cards, appointment reminders, and patient education materials should include the provider’s name, credentials, and role. For example, a business card might read:
[Name] , DNP, APRN
Doctor of Nursing Practice
Board-Certified Nurse Practitioner
5.3 Signage
Signage in the clinical setting should also clearly identify DNPs and their roles. This can include nameplates on doors, signage in waiting rooms, and information on the practice website. The signage should use clear and concise language to explain the provider’s qualifications and role.
5.4 Electronic Health Records (EHRs)
Electronic health records (EHRs) should clearly identify DNPs and their credentials. This ensures that all members of the healthcare team are aware of the provider’s role and qualifications. EHRs should also include a way for patients to easily access information about their providers, including their credentials and training.
6. Addressing Patient Confusion
Despite efforts to promote transparency, some patients may still be confused about the role and qualifications of DNPs. It is essential to address this confusion proactively and provide patients with accurate information.
6.1 Educating Patients
Healthcare providers should take the time to educate patients about the different types of healthcare professionals and their roles. This can be done through verbal explanations, written materials, and online resources. Patients should understand the education, training, and scope of practice of DNPs and how they differ from medical doctors.
6.2 Answering Questions
Patients should be encouraged to ask questions about their healthcare providers and their treatment plans. Healthcare providers should be prepared to answer these questions in a clear and understandable manner. If a patient expresses confusion about the provider’s role or qualifications, the provider should take the time to explain their credentials and how they contribute to the patient’s care.
6.3 Providing Resources
Healthcare providers should provide patients with resources that can help them learn more about DNPs and their role in healthcare. This can include websites, brochures, and articles from reputable sources. By providing patients with access to accurate information, healthcare providers can empower them to make informed decisions about their care.
7. The Future Of Nursing Practice
The role of nurse practitioners is evolving rapidly, driven by factors such as the growing demand for healthcare services, the aging population, and the increasing complexity of medical care. As the healthcare landscape continues to change, DNPs will play an increasingly important role in delivering high-quality, cost-effective care to patients across diverse settings.
7.1 Expanding Scope Of Practice
Many states are considering legislation to expand the scope of practice for nurse practitioners, allowing them to practice independently without physician oversight. Proponents of this expansion argue that it will increase access to care, reduce healthcare costs, and improve patient outcomes. Opponents, however, raise concerns about patient safety and the quality of care.
7.2 Increasing Demand For DNPs
The demand for DNPs is expected to grow significantly in the coming years, driven by the factors mentioned above. As the population ages and the demand for healthcare services increases, DNPs will be needed to fill critical gaps in the healthcare workforce. This will create new opportunities for DNPs in a variety of settings, including hospitals, clinics, private practices, and community health centers.
7.3 Advancing The Nursing Profession
The DNP degree is helping to advance the nursing profession by preparing nurses for leadership roles in clinical practice, education, and research. DNP graduates are equipped with the knowledge and skills to lead healthcare teams, translate research into practice, and advocate for policies that improve patient care. As more nurses pursue DNP degrees, the nursing profession will continue to evolve and contribute to the advancement of healthcare.
8. Case Studies
Looking at real-world examples can provide a clearer understanding of the complexities surrounding the use of the title “Doctor” by DNPs and its impact on patient care.
8.1 Case Study 1: Rural Health Clinic
- Scenario: A DNP working in a rural health clinic introduces herself as “Doctor” to patients.
- Ethical Considerations: Patients may assume the DNP is a medical doctor, leading to potential misunderstandings about the provider’s qualifications and scope of practice.
- Transparency Solution: The DNP should clearly state, “I’m Dr. [Name], a Doctor of Nursing Practice and a certified nurse practitioner.”
- Outcome: Patients understand the DNP’s role and qualifications, leading to increased trust and effective communication.
8.2 Case Study 2: Urban Hospital
- Scenario: A patient with multiple chronic conditions is being treated by a team of healthcare providers, including a DNP who uses the title “Doctor.”
- Coordination Challenges: Other healthcare professionals may assume the DNP is a physician, leading to potential confusion in care coordination.
- Clarity Solution: The hospital implements a policy requiring all DNPs to use their full credentials (e.g., Dr. [Name], DNP, APRN) in verbal and written communications.
- Outcome: Improved communication and coordination among the healthcare team, resulting in better patient outcomes.
8.3 Case Study 3: Academic Setting
- Scenario: A DNP professor in a university setting uses the title “Doctor” while teaching nursing students.
- Educational Context: Students may not understand the difference between a DNP and a medical doctor, leading to potential misconceptions about the roles and responsibilities of each.
- Educational Strategy: The professor incorporates a lesson on the various types of healthcare professionals and their qualifications into the curriculum.
- Outcome: Students develop a clear understanding of the different roles within the healthcare system, promoting interprofessional collaboration and respect.
9. Expert Opinions
Hearing from experts in the field can provide valuable insights into the ongoing discussion about the use of the title “Doctor” by DNPs and its implications for healthcare.
9.1 Dr. Joyce Johnson, PhD, RN, FAAN
- Professor of Nursing, University of California, San Francisco
- “As DNPs become more prevalent in healthcare, it’s essential to ensure that patients understand their qualifications and scope of practice. Transparency is key to building trust and promoting informed decision-making.”
9.2 Dr. Michael Smith, MD, MPH
- Chief Medical Officer, Community Health Center Network
- “While I respect the education and training of DNPs, I believe it’s important to avoid any confusion with medical doctors. Using the full credentials (e.g., Dr. [Name], DNP, APRN) is the best way to ensure clarity.”
9.3 Dr. Emily Brown, DNP, APRN
- President, American Association of Nurse Practitioners
- “DNPs have earned the right to use the title ‘Doctor,’ but we must do so responsibly. We need to be proactive in educating patients about our roles and qualifications to avoid any misunderstandings.”
10. Resources For Further Information
Accessing reliable sources of information can help healthcare professionals, patients, and policymakers stay informed about the evolving role of DNPs in healthcare.
10.1 Professional Organizations
- American Association of Nurse Practitioners (AANP)
- https://www.aanp.org/
- Provides resources, education, and advocacy for nurse practitioners.
- National Council of State Boards of Nursing (NCSBN)
- https://www.ncsbn.org/
- Offers information on nursing regulation and scope of practice.
- American Nurses Association (ANA)
- https://www.nursingworld.org/
- Advocates for the nursing profession and provides resources for nurses.
10.2 Government Agencies
- National Institutes of Health (NIH)
- https://www.nih.gov/
- Conducts and supports medical research.
- Centers for Disease Control and Prevention (CDC)
- https://www.cdc.gov/
- Provides health information and promotes disease prevention.
- Health Resources and Services Administration (HRSA)
- https://www.hrsa.gov/
- Works to improve healthcare access for underserved populations.
10.3 Academic Institutions
- Schools of Nursing
- Many universities offer DNP programs and conduct research on nursing practice.
- Examples: Johns Hopkins School of Nursing, Duke University School of Nursing.
10.4 Publications
- Journal of the American Association of Nurse Practitioners
- Nursing Outlook
- The Nurse Practitioner
FAQ Section
Here are ten frequently asked questions (FAQs) about nurse practitioners and their use of the title “Doctor,” designed to provide clarity and address common concerns.
1. What is the difference between a Nurse Practitioner (NP) and a Medical Doctor (MD)?
An NP is an advanced practice registered nurse who has completed a master’s or doctoral degree program, while an MD is a physician who has completed medical school and residency training. NPs focus on holistic, patient-centered care, while MDs have a broader scope of practice and often specialize in specific areas of medicine.
2. Can a Nurse Practitioner prescribe medication?
Yes, Nurse Practitioners can prescribe medication in all 50 states, though the extent of their prescribing authority may vary depending on state laws. They can prescribe a wide range of medications, including controlled substances, to treat various medical conditions.
3. What is a Doctor of Nursing Practice (DNP)?
A DNP is a terminal degree in nursing, representing the highest level of education for nurse practitioners and other advanced practice registered nurses. DNP programs focus on equipping nurses with the knowledge and skills to improve healthcare outcomes through evidence-based practice and leadership.
4. Is it legal for a DNP to call themselves “Doctor”?
Yes, it is generally legal for a DNP to use the title “Doctor,” as they have earned a doctoral degree. However, they must ensure that they clearly communicate their credentials and role to patients to avoid confusion and maintain transparency.
5. How should a DNP introduce themselves in a clinical setting?
A DNP should introduce themselves by stating their name, credentials, and role. For example, they might say, “Hello, my name is Dr. [Name], and I am a Doctor of Nursing Practice and a board-certified nurse practitioner.”
6. What are the ethical considerations for DNPs using the title “Doctor”?
The ethical considerations include ensuring that patients are not misled into thinking that the DNP is a medical doctor and maintaining transparency about their qualifications and scope of practice.
7. How can healthcare organizations ensure transparency when DNPs use the title “Doctor”?
Healthcare organizations can implement policies requiring DNPs to use their full credentials in verbal and written communications, provide patient education materials explaining the roles of different healthcare professionals, and clearly display DNPs’ credentials on signage and electronic health records.
8. What are the benefits of having DNPs in the healthcare system?
DNPs play a vital role in expanding access to quality healthcare, particularly in underserved areas. They provide comprehensive care, including diagnosing and treating illnesses, prescribing medications, and ordering diagnostic tests, often at a lower cost than physicians.
9. How is the scope of practice for NPs determined?
The scope of practice for NPs is determined by state laws and regulations. Some states have full practice authority, allowing NPs to practice independently, while others require physician supervision or collaboration.
10. Where can I find more information about Nurse Practitioners and DNPs?
You can find more information about Nurse Practitioners and DNPs from professional organizations such as the American Association of Nurse Practitioners (AANP) and the National Council of State Boards of Nursing (NCSBN), as well as government agencies like the National Institutes of Health (NIH) and academic institutions offering DNP programs.
Conclusion
The question of whether a nurse practitioner can call themselves “doctor” is complex, with legal, ethical, and practical considerations. Ultimately, transparency and clear communication are essential for ensuring that patients understand the qualifications and role of their healthcare providers. By adhering to ethical guidelines, complying with legal regulations, and educating patients, DNPs can use the title “doctor” responsibly and contribute to the delivery of high-quality, patient-centered care.
At thebootdoctor.net, we are committed to providing accurate and reliable information about healthcare professionals and practices. We encourage you to explore our website for more resources and insights on healthcare topics. If you’re in Houston, we invite you to visit us at 6565 Fannin St, Houston, TX 77030, United States, or call us at +1 (713) 791-1414 for personalized advice and care. We are dedicated to helping you make informed decisions about your health and well-being.
 Nurse Practitioner
Nurse Practitioner
Alt Text: A female nurse practitioner smiles confidently while assisting a senior patient with her walker in a bright, modern clinic setting, emphasizing compassionate patient care and accessibility.
 Advanced Practice Registered Nurses Advice
Advanced Practice Registered Nurses Advice
Alt Text: An infographic from the Texas Nurse Practitioners Office provides clear advice on how advanced practice registered nurses should accurately represent themselves to patients, ensuring transparency and preventing confusion.
 Minnesota Statutes Regarding Use of the Title “Doctor” in Clinical Settings
Minnesota Statutes Regarding Use of the Title “Doctor” in Clinical Settings
Alt Text: A document outlining Minnesota statutes concerning the appropriate use of the title “Doctor” in clinical settings by advanced practice registered nurses, highlighting the importance of clear identification and patient safety.

