Are doctors notified when you fill a prescription? Yes, doctors can indeed find out if you’ve filled a prescription, primarily through Electronic Health Records (EHR) and prescription monitoring programs. At thebootdoctor.net, we aim to provide clear and reliable information to help you understand how your healthcare is managed, ensuring you feel informed and empowered when it comes to your health, offering solutions for foot health and beyond. Continue reading to learn more about medical adherence, patient privacy, and prescription history.
1. What is an Electronic Health Record (EHR)?
An Electronic Health Record (EHR) is a real-time, patient-centered record that makes information available instantly and securely to authorized users. EHRs contain a patient’s medical history, diagnoses, medications, treatment plans, immunization dates, allergies, radiology images, and laboratory and test results.
EHRs provide healthcare providers with tools to make informed decisions about a patient’s care and streamline workflows by automating processes. According to HealthIT.gov, one of the key features of an EHR is that health information can be created and managed by authorized providers in a digital format capable of being shared with other providers across more than one healthcare organization. This comprehensive view of a patient’s medical history ensures coordinated and effective care.
Here’s a sample of an EHR on-screen Record.
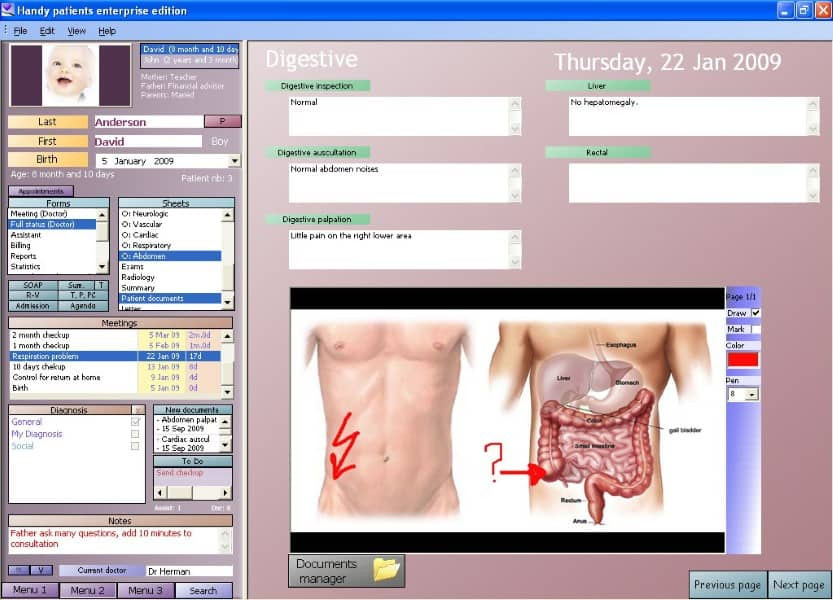 electronic health record sample
electronic health record sample
1.1. What Information Does an EHR Typically Include?
EHRs compile data from various healthcare providers involved in a patient’s care, including emergency facilities, laboratories, specialists, medical imagery providers, pharmacies, and work and school medical clinics. This comprehensive approach ensures that all relevant health information is accessible to those who need it.
The data stored in an EHR typically includes:
- Medical History: A detailed account of past illnesses, surgeries, and treatments.
- Diagnoses: Current and past medical conditions.
- Medications: A list of prescribed medications, dosages, and administration routes.
- Treatment Plans: Outlines of recommended treatments and therapies.
- Immunization Dates: Records of vaccinations and immunizations.
- Allergies: Information about known allergies and adverse reactions.
- Radiology Images: X-rays, MRIs, and other medical imaging results.
- Laboratory and Test Results: Data from blood tests, urine tests, and other diagnostic procedures.
1.2. How Does EHR Access Benefit Healthcare Providers?
Having immediate access to this information enables healthcare providers to make informed decisions, reduce errors, and improve patient outcomes. The ability to share information across different healthcare settings ensures continuity of care, which is especially important for patients with chronic conditions or those who require specialized treatment.
Benefits of EHR access for healthcare providers include:
- Improved Decision-Making: Access to comprehensive patient data allows for more informed and accurate diagnoses and treatment plans.
- Reduced Errors: Electronic records minimize the risk of errors associated with handwritten notes and manual data entry.
- Enhanced Coordination of Care: Sharing information across different healthcare settings ensures that all providers are aware of a patient’s medical history and current treatment plan.
- Streamlined Workflows: Automating processes and reducing paperwork allows healthcare providers to focus more on patient care.
- Better Patient Outcomes: By facilitating more effective and coordinated care, EHRs contribute to improved patient health outcomes.
2. How Do Pharmacies Retain Prescription Records?
Pharmacies are required to maintain detailed records of prescriptions to ensure patient safety and regulatory compliance. The length of time these records are kept can vary depending on state and federal laws, but generally, pharmacies retain prescription records for several years. This allows pharmacists to track medication usage, monitor for potential drug interactions, and provide accurate information to healthcare providers.
2.1. Guidelines for Prescription Record Retention
The guidelines for how long pharmacies must keep medical records, including prescriptions, are outlined in simple terms below:
| Record Type | Description/Information Contained | Retention Period |
|---|---|---|
| Prescriptions | A hard copy or electronic record of a prescription | 42 months (3.5 years), or 2 years past the completion of therapy, depending on the specific regulations |
| Patient Record | Demographics, Drug Profile, Record of Care Provided | 10 Years past the last date of Pharmacy Service Provided or 2 years past age of Majority, depending on the specific regulations |
| Record of Care | Drug therapy, problems, interventions & Monitoring, Prescriptions NOT Filled | 10 Years past the last date of Pharmacy Service Provided or 2 years past the age of majority |
| Drug Error | Incidents, adverse drug effects, adverse outcomes | 10 years after the error is discovered |
| Health Info Disclosure | Records of diagnosis, treatment, and care shared with other health organizations | 10 years following the date of disclosure |
| Narcotic Receipts | Records of narcotics received at a pharmacy or licensed outlet, such as a wholesaler | 2 years from the date of the receipt |
2.2. E-Prescriptions and Doctor Notifications
When a physician sends a prescription electronically to a pharmacy, it’s referred to as an “e-Prescription” or “e-Rx.” E-Rx programs often allow doctors to receive notifications indicating whether the prescription has been picked up, not picked up, or partially filled. This immediate feedback helps doctors monitor patient adherence and follow up as necessary.
E-prescribing offers several advantages over traditional paper prescriptions:
- Increased Efficiency: E-prescriptions are transmitted directly to the pharmacy, reducing the risk of lost or illegible prescriptions.
- Improved Accuracy: Electronic prescribing systems can alert doctors to potential drug interactions and allergies, helping to prevent medication errors.
- Enhanced Patient Safety: Real-time monitoring of prescription fills allows doctors to identify and address potential issues with patient adherence.
3. What Other Ways Can Doctors Track Your Medication?
Beyond EHRs and e-prescriptions, doctors can track your medication through prescription drug monitoring programs (PDMPs) and direct communication with pharmacies. These methods provide additional layers of oversight to ensure patient safety and prevent drug misuse.
3.1. Prescription Drug Monitoring Programs (PDMPs)
More than three dozen states in the U.S. have established databases to track prescriptions for opioid and narcotic drugs. These databases monitor doctors’ prescription-writing, pharmacy prescription-dispensing, and patients’ prescription filling.
When a patient visits their doctor and there’s a possibility of prescribing a pain-relieving drug, the doctor can access the database to ensure the patient isn’t “doctor shopping” to amass more prescription drugs than legally or medically entitled to. This system helps prevent potential overdoses and ensures that patients receive appropriate care.
PDMPs offer numerous benefits:
- Reduced Doctor Shopping: By tracking prescriptions across different providers, PDMPs help prevent patients from obtaining multiple prescriptions for the same medication.
- Prevention of Overdoses: Monitoring prescription fills allows doctors to identify patients who may be at risk of overdose and intervene as necessary.
- Improved Prescribing Practices: PDMPs provide doctors with data on their prescribing patterns, helping them to identify areas where they can improve their practices.
3.2. Discussions to Share Information Across State Lines
Discussions are underway to make sharing this information possible across state lines, which would further prevent patients from doctor shopping in other states. This enhanced coordination would provide a more complete picture of a patient’s prescription history, leading to better-informed prescribing decisions.
Sharing prescription data across state lines can address several challenges:
- Mobility of Patients: Patients who move frequently may obtain prescriptions from different states, making it difficult to track their medication usage.
- Border Shopping: Patients may cross state lines to obtain prescriptions in states with less stringent regulations.
- Comprehensive Data: A national database would provide a more complete and accurate picture of a patient’s prescription history, regardless of where they receive care.
3.3. Benefits of Medication Tracking
While some patients may be concerned that such databases violate their privacy, there are important reasons to support the use of these tools. Doctors can more confidently prescribe drugs for appropriate patients at appropriate times, with less fear of legal trouble. Emergency room personnel can access these databases to avoid prescribing conflicting drugs or dismissing patients due to their pain medication history.
Key benefits of medication tracking include:
- Confident Prescribing: Doctors can prescribe medications with greater confidence, knowing that they have access to a patient’s complete prescription history.
- Reduced Legal Risks: Access to PDMPs can help doctors avoid legal issues related to inappropriate prescribing practices.
- Improved Emergency Care: Emergency room personnel can make better-informed decisions about patient care by accessing prescription drug information.
4. Why Don’t People Fill Their Prescriptions?
According to the National Center for Biotechnology Information (NCBI), approximately 50% of patients do not take their medications as prescribed. Understanding the reasons behind this can help healthcare providers address the issues and improve patient adherence.
There are numerous reasons why people may not fill their prescriptions. Let’s explore some of the most common ones:
4.1. Cost
Patients may not fill prescriptions due to affordability issues. They might reduce their medication intake to extend their supply. For those struggling with medication costs, resources like Prescription Hope can offer assistance.
4.2. Fear
Potential side effects can deter patients from filling prescriptions, especially if they have heard negative stories about the medication’s effectiveness or experienced adverse reactions in the past.
4.3. Misunderstanding
Patients may not understand the necessity of the medication for improving their health, particularly those with chronic illnesses who don’t experience immediate relief. This lack of understanding can lead to premature discontinuation of the medication.
4.4. Too Many Medications
The greater the variety of prescribed medications and the higher the dosing frequency, the more likely a patient is to be non-adherent. Managing multiple medications can be overwhelming and lead to missed doses or confusion.
4.5. Lack of Symptoms
If symptoms disappear, patients may believe the illness has ended and see little need to continue with medication. It’s important for patients to understand that some medications are designed to prevent symptoms from returning, and discontinuing them can lead to a relapse.
4.6. Denial
Some patients believe their condition will resolve on its own, negating the need for medication. This denial can stem from a lack of understanding about the severity of their condition or a preference for alternative treatments.
4.7. Worry
Dependency can be a concern, making patients reluctant to start medications they fear becoming dependent on, contributing to non-adherence. Addressing these concerns and providing reassurance can help patients feel more comfortable with their treatment plan.
4.8. Depression
Depression can diminish the importance placed on health issues, making patients less likely to fill their prescriptions. Mental health plays a significant role in medication adherence, and addressing underlying mental health issues can improve outcomes.
4.9. Mistrust
Patients may distrust their doctor’s diagnosis or motives for prescribing certain medications, possibly due to personal beliefs or media reports about pharmaceutical companies. Building trust and open communication between patients and healthcare providers can help alleviate these concerns.
4.10. The Importance of Communication
According to Dr. Michael A. Fischer of Brigham and Women’s Hospital in Boston, “If they do not fully understand the reason that they’re being prescribed the medication, they may be less likely to take it.” He advises patients to ask their doctors directly if they are unsure why they are being prescribed a medication.
Open communication between patients and doctors is essential for ensuring medication adherence. Patients should feel comfortable asking questions, expressing concerns, and seeking clarification about their treatment plans.
5. What Are The Consequences of Not Filling Your Prescription?
Not filling prescriptions can have significant consequences for both individual health and the economy. Understanding these consequences can motivate patients to adhere to their prescribed medication regimens.
5.1. Medical Non-Adherence
According to a study by The National Council on Patient Information and Education, as many as half of all patients do not follow their doctors’ advice when it comes to medications. Non-adherence can lead to increased illness, higher mortality rates, and more complications, especially for those with chronic diseases like high blood pressure and diabetes.
5.2. Economic Impact
The overall cost of medication non-adherence is staggering, amounting to more than $170 billion each year in the United States alone, with some reports estimating the figure as high as $300 billion. These costs include increased hospitalizations, emergency room visits, and other healthcare expenses.
5.3. Recent Research on Medical Non-Adherence
Much of the research on non-adherence has focused on patients who have filled their prescriptions, examining whether they come back for refills and regularly take their medication. However, with better-tracking systems and more healthcare providers using electronic medical records, it has been discovered that non-adherence may begin even before the patient fills their prescription.
5.4. Primary Non-Adherence
Research from Harvard Medical School published the largest study to date on “primary nonadherence” and found that more than 20% of first-time patient prescriptions were never filled. First-time prescriptions for chronic diseases like high cholesterol, high blood pressure, and diabetes were more likely not to be filled, whereas those for pediatric patients 18 years of age and younger and for antibiotics were more likely to be filled.
Understanding the complexities and impacts of non-adherence is vital for improving healthcare outcomes.
6. Understanding the Nuances of Patient Privacy
While doctors have several ways to check if you’ve filled a prescription, it’s essential to know that patient privacy is still a priority. Your medical information is protected by laws like the Health Insurance Portability and Accountability Act (HIPAA), which sets rules for who can access your health data and how it can be used.
6.1. HIPAA and Your Prescription Information
HIPAA gives you rights over your health information, including the right to see and get a copy of your records, as well as the right to request corrections if something is wrong. It also limits who can see your health information without your permission. Generally, your doctor needs your permission to share your prescription history with others, unless it’s for treatment, payment, or healthcare operations.
6.2. Exceptions to Privacy Rules
There are some exceptions to these privacy rules. For example, doctors can share your prescription information with other healthcare providers involved in your care without your explicit permission. They can also share it with pharmacies to fill your prescriptions, and with insurance companies to process your claims. Additionally, law enforcement agencies can access your prescription information if they have a valid court order.
6.3. Your Role in Protecting Your Privacy
You also have a role to play in protecting your privacy. Be careful about who you share your health information with, and always read the privacy policies of healthcare providers and pharmacies. If you have concerns about how your information is being used, talk to your doctor or a privacy advocate.
7. The Doctor-Patient Relationship: Trust and Transparency
The ability for doctors to see if you’ve filled a prescription can play a role in the doctor-patient relationship. It can help doctors get a better understanding of your health and make more informed decisions about your care. However, it can also create a sense of unease or distrust if you’re not aware that your doctor has access to this information.
7.1. Building Trust Through Open Communication
The key to a healthy doctor-patient relationship is open communication and trust. Be honest with your doctor about your medications, and ask questions if you’re unsure about something. Your doctor should also be transparent about how they use your prescription information and explain why it’s important for your care.
7.2. Benefits of Transparency
When you trust your doctor and feel comfortable sharing information with them, it can lead to better health outcomes. Your doctor can get a more complete picture of your health, which can help them make more accurate diagnoses and recommend the most effective treatments.
7.3. Addressing Concerns
If you have concerns about your doctor’s access to your prescription information, talk to them about it. They can explain why they need this information and how they use it to improve your care. If you’re still not comfortable, you can seek a second opinion or find a new doctor.
8. Frequently Asked Questions (FAQs)
Here are some frequently asked questions related to doctors being notified when you fill a prescription:
8.1. Can my doctor see all the medications I’m taking?
Yes, through EHRs and PDMPs, your doctor can typically see all the medications you’ve been prescribed, including those from other doctors.
8.2. Will my doctor know if I don’t fill a prescription?
Yes, doctors can receive notifications if you don’t pick up an e-prescription, and they can also see unfilled prescriptions in your medical records.
8.3. Is my prescription information kept private?
Yes, your prescription information is protected by laws like HIPAA, which limit who can access your health data without your permission.
8.4. What if I don’t want my doctor to see my prescription history?
While it’s generally beneficial for your doctor to have a complete picture of your health, you can discuss your concerns with them and explore options for limiting access to your prescription history.
8.5. How can I access my prescription history?
You have the right to see and get a copy of your medical records, including your prescription history, from your doctor or pharmacy.
8.6. Are over-the-counter medications included in my prescription record?
No, over-the-counter medications are not typically included in your prescription record, as they don’t require a prescription from a doctor.
8.7. Can my insurance company see if I filled a prescription?
Yes, your insurance company can see if you filled a prescription, as they need this information to process your claims.
8.8. What should I do if I can’t afford my medications?
Talk to your doctor about potential alternatives or resources like Prescription Hope that can help you save money on your medications.
8.9. Can my employer see my prescription history?
No, your employer cannot access your prescription history without your permission, as this is protected by HIPAA and other privacy laws.
8.10. How long do pharmacies keep my prescription records?
Pharmacies typically keep prescription records for several years, as required by state and federal laws.
9. Foot Health and Medication: A Critical Connection
At thebootdoctor.net, we focus on foot health, which can often be intertwined with medication management. For example, individuals with diabetes need to manage their blood sugar levels through medication to prevent foot complications. Similarly, those with arthritis may take medications to reduce inflammation and pain, improving their ability to walk and stay active.
9.1. Diabetes and Foot Care
Diabetes can lead to nerve damage (neuropathy) and poor circulation, increasing the risk of foot ulcers and infections. Proper medication management is crucial for controlling blood sugar levels and preventing these complications. Regular foot exams and proper foot care are also essential for individuals with diabetes.
9.2. Arthritis and Mobility
Arthritis can cause pain and stiffness in the joints of the feet, making it difficult to walk and perform daily activities. Medications such as anti-inflammatory drugs and pain relievers can help manage these symptoms and improve mobility. Supportive footwear and orthotics can also provide additional comfort and support.
9.3. Addressing Foot Pain
Many people experience foot pain due to various conditions, such as plantar fasciitis, bunions, and hammertoes. Medications like pain relievers and anti-inflammatory drugs can help alleviate pain and inflammation. Additionally, treatments like physical therapy, orthotics, and injections may be recommended to address the underlying cause of the pain.
10. The Role of thebootdoctor.net in Your Healthcare Journey
At thebootdoctor.net, we are committed to providing you with reliable and easy-to-understand information about foot health and overall wellness. We understand that managing your health can be complex, and we strive to empower you with the knowledge and resources you need to make informed decisions.
10.1. Expert Resources and Guidance
Our website offers a wealth of articles, guides, and resources on various foot conditions, treatments, and preventative measures. We collaborate with experienced podiatrists and healthcare professionals to ensure that our content is accurate, up-to-date, and relevant to your needs.
10.2. Supportive Community
We also foster a supportive community where you can connect with others, share your experiences, and ask questions. Our forums and social media channels provide a safe and welcoming space for you to engage with fellow readers and learn from their insights.
10.3. Encouragement to Seek Professional Advice
While we strive to provide you with valuable information, it’s important to remember that our website is not a substitute for professional medical advice. Always consult with a qualified healthcare provider for any health concerns or before making any decisions related to your treatment or care.
Conclusion
Understanding how doctors access your prescription information can empower you to take control of your health and well-being. While privacy is a priority, these tracking methods help ensure patient safety and improve healthcare outcomes. If you’re seeking more information on foot health or need expert advice, visit thebootdoctor.net today. Explore our articles, connect with our community, and take the first step towards healthier feet. Our address is 6565 Fannin St, Houston, TX 77030, United States. You can also reach us by phone at +1 (713) 791-1414. Let us be your trusted resource for all things foot-related!
