With its crisp, clean appearance, the white doctor coat is instantly recognizable and deeply symbolic. Beyond its practical function, this garment carries significant weight, representing different things to patients, physicians, and the healthcare community at large. Once a clear marker distinguishing evidence-based practitioners from dubious healers, the white coat’s meaning has become increasingly complex in modern medicine.
A Garment Rooted in Professionalism and Trust
The adoption of white lab coats by surgeons and physicians in the late 19th century marked a turning point in medical history. This shift was intentional, designed to visually separate trained professionals from those practicing questionable medicine. The white coat became a symbol of the burgeoning scientific approach to healthcare, representing a commitment to hygiene and evidence-based practice.
Today, for many, the white coat continues to evoke feelings of professionalism, integrity, and dedication to patient care. It signifies expertise and a serious commitment to alleviating suffering. A survey conducted by the University of Michigan, the largest of its kind, involving 4,000 patients across 10 U.S. academic medical centers, underscored this perception. The study revealed that patients viewed doctors wearing white coats over business attire as more knowledgeable, trustworthy, caring, and approachable. This was especially true for patients aged 65 and older. Doctors in scrubs with a white coat also scored highly, further emphasizing the positive impact of the white coat on patient perception.
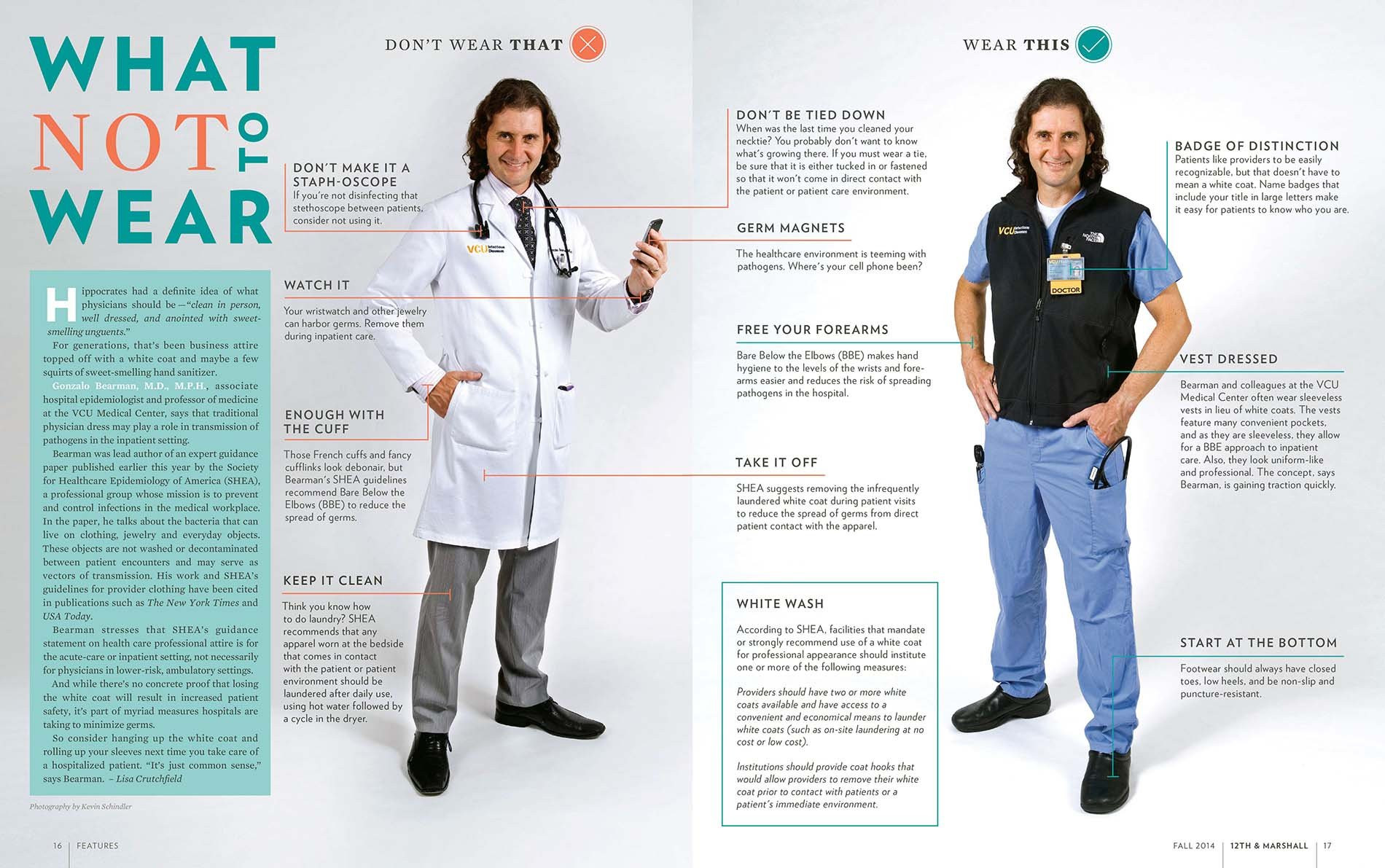 A doctor in two different outfits, one with a white coat and one without, demonstrating professional attire options
A doctor in two different outfits, one with a white coat and one without, demonstrating professional attire options
The Controversy: Germs, Barriers, and Evolving Perceptions
Despite its positive connotations, the white coat is not without its critics. Some argue that it represents elitism and can create an unnecessary barrier between doctors and patients. Pediatricians and psychiatrists, for instance, have often opted to forgo white coats, recognizing that they can be intimidating, particularly to younger or more vulnerable patients. The Mayo Clinic even advises its physicians to wear business attire alone, aiming to foster a more relaxed and approachable doctor-patient relationship.
Furthermore, a significant concern has emerged regarding hygiene. Numerous studies have demonstrated that white coats can harbor potentially harmful microbes, especially around the cuffs and pockets. Research dating back to the early 1990s has consistently shown the presence of bacteria on white coats. This has led to discussions and even policy changes, such as the UK’s National Health Service recommending bare-elbows for doctors who choose to wear white coats. The American Medical Association also considered the possibility of banning white coats in hospitals due to hygiene concerns.
Balancing Image with Infection Control
While the image of a doctor in a white coat may inspire confidence, the reality of potential infection risks cannot be ignored. Some argue that more frequent laundering of white coats could mitigate these risks. However, studies have shown that doctors may launder their coats infrequently.
Infectious disease specialists, while acknowledging the need for caution, point out that there is no definitive evidence directly linking white coat contamination to patient infections. Instead, practical solutions like rolling up sleeves or adopting short-sleeved coats are gaining traction. A 2017 study highlighted that long sleeves contribute to cross-contamination, suggesting short sleeves as a more hygienic alternative.
Dr. Amrita John, an infectious disease specialist, advocates for short-sleeved coats as a practical compromise, balancing the traditional expectation of a white coat with the need for infection control. This approach acknowledges the symbolic importance of the coat while prioritizing patient safety.
Innovations and Alternatives: Rethinking Doctor’s Attire
Recognizing the complexities surrounding the white coat, some institutions are exploring innovative alternatives. Virginia Commonwealth University School of Medicine, for example, has introduced sleeveless black neoprene vests for doctors. These vests offer the practicality of pockets and warmth without the hygiene concerns associated with sleeves. The black color, chosen to align with university colors, provides a professional appearance while moving away from the traditional white.
This move towards alternatives also addresses “white coat syndrome,” a phenomenon where anxiety related to doctors can cause elevated blood pressure readings. Research suggests that this syndrome is not benign and may be linked to increased mortality risk. More relaxed or less formal attire might help reduce patient anxiety and improve the accuracy of physiological measurements.
The Shifting Hierarchy and Future of the White Coat
Even within the tradition of white coats, hierarchies have existed, notably in the length of the coat signifying experience level. First-year residents traditionally wear shorter, hip-length coats, while more senior residents and doctors wear longer, knee-length coats. However, this tradition is also being questioned.
The Osler Medical Residency Training Program at Johns Hopkins Hospital, a historically significant program, has abandoned the practice of short white coats for first-year residents. The decision came in response to feedback from new doctors who felt the shorter coat symbolized an unnecessary hierarchy. This change reflects a move towards a more egalitarian approach in medical training, prioritizing collaboration and open communication over rigid symbols of rank.
While the white coat may not disappear entirely, its role and perception are undoubtedly evolving. Personal preference, patient expectations, hygiene concerns, and the desire for a more approachable and egalitarian healthcare environment are all contributing to an ongoing discussion about the future of doctor’s attire. Ultimately, the focus remains on providing the best possible patient care, and the white coat, or its alternatives, must serve that primary goal.
