Are you concerned about a painful lump on your skin and wondering when to seek medical help? When To See A Doctor About A Boil is crucial to understand for proper care and to avoid complications; thebootdoctor.net offers reliable information and guidance to help you make informed decisions. Addressing this issue promptly ensures effective treatment and promotes overall skin health, helping you find relief and clarity in managing skin infections and potential medical interventions.
1. What Is A Boil?
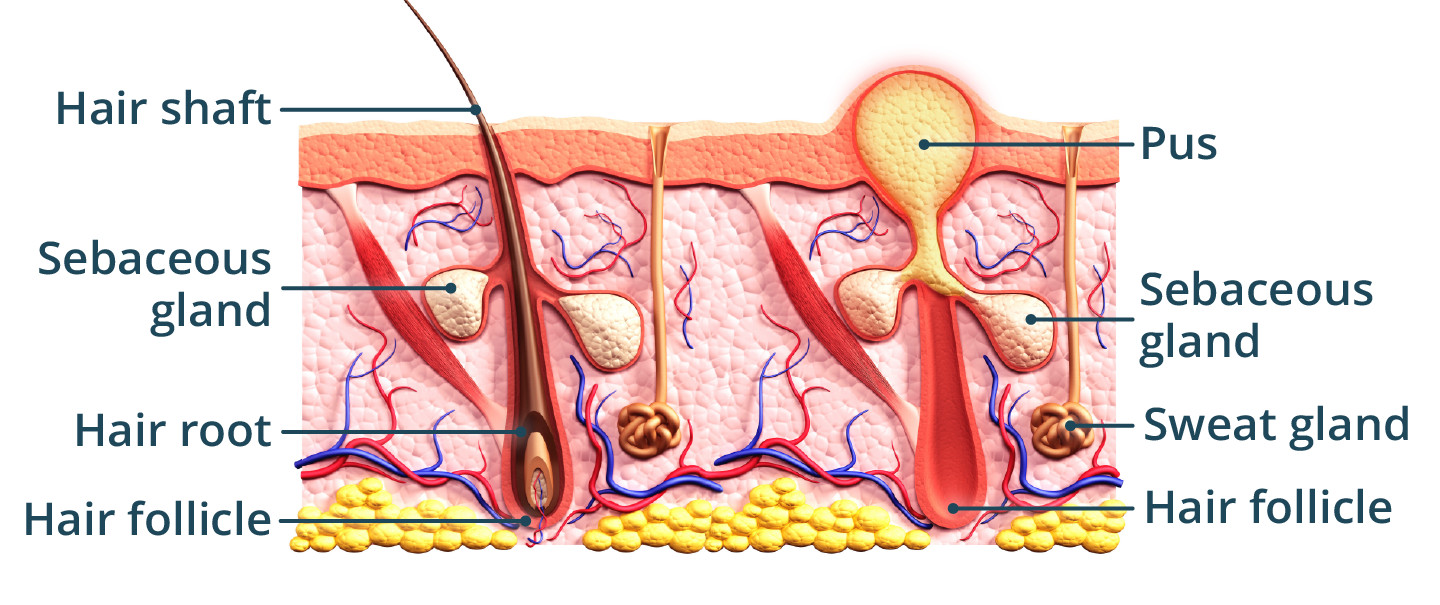
A boil is a painful, pus-filled bump that forms under your skin when bacteria infects one or more hair follicles. Often caused by Staphylococcus aureus bacteria, boils typically start as small, red bumps and progressively enlarge as they fill with pus. Understanding what a boil is can help you recognize the symptoms and know when to seek medical advice.
1.1. Furuncles vs. Carbuncles: Understanding the Difference
- Furuncle: A furuncle, commonly known as a boil, is an infection of a single hair follicle.
- Carbuncle: A carbuncle is a cluster of boils connected beneath the skin. Carbuncles are more severe infections and require medical attention.
| Feature | Furuncle (Boil) | Carbuncle |
|---|---|---|
| Definition | Infection of a single hair follicle | Cluster of boils connected beneath the skin |
| Severity | Less severe | More severe |
| Number of Sites | Single site of infection | Multiple interconnected sites of infection |
| Medical Attention | Often treatable at home | Typically requires medical intervention (antibiotics, drainage) |
| Symptoms | Localized pain and swelling | Fever, fatigue, and more widespread inflammation |
| Scarring | Minimal scarring | Higher risk of significant scarring |
Understanding the differences between furuncles and carbuncles can help you determine the severity of your condition and the appropriate course of action. If you suspect you have a carbuncle, it’s essential to seek medical attention promptly.
1.2. Common Locations for Boils
Boils can appear anywhere on the body but are more common in areas with hair and where friction occurs. These areas include:
- Face
- Neck
- Armpits
- Groin
- Buttocks
- Inner thighs
These locations are prone to boils due to increased sweating and friction, which can create an environment conducive to bacterial growth.
2. Recognizing the Symptoms of a Boil
Identifying the symptoms of a boil is crucial for timely intervention. Common symptoms include:
- Red, Tender Lump: A painful, red bump on the skin is usually the first sign.
- Increasing Size: The lump typically grows larger over several days as it fills with pus.
- Pain: The area around the boil can be tender and painful to the touch.
- White or Yellow Center: As the boil matures, a white or yellow pus-filled center becomes visible.
- Surrounding Swelling: The skin around the boil may become swollen and inflamed.
- Fever: In more severe cases, especially with carbuncles, you may experience fever and fatigue.
Being able to recognize these symptoms will help you decide when to seek professional medical advice.
3. What Causes Boils?
Boils are primarily caused by bacterial infections, most commonly Staphylococcus aureus. These bacteria can enter the body through:
- Breaks in the Skin: Cuts, scrapes, or insect bites can provide entry points for bacteria.
- Hair Follicles: Bacteria can infect hair follicles, leading to inflammation and pus formation.
- Poor Hygiene: Inadequate hygiene can increase the risk of bacterial infections.
- Weakened Immune System: Conditions that weaken the immune system can make you more susceptible to boils.
- Underlying Skin Conditions: Conditions like eczema can compromise the skin’s barrier, increasing the risk of infection.
3.1. Risk Factors That Increase Susceptibility
Certain factors can increase your risk of developing boils:
- Close Contact with Infected Individuals: Sharing towels, razors, or clothing with someone who has a boil can spread the infection.
- Diabetes: High blood sugar levels can impair immune function and increase the risk of skin infections.
- Obesity: Skin folds can create moist environments where bacteria thrive.
- Compromised Immune System: Conditions like HIV/AIDS or treatments like chemotherapy can weaken the immune system.
- Poor Hygiene: Not washing regularly or keeping wounds clean can increase the risk of infection.
- Skin Conditions: Pre-existing skin conditions, such as eczema and dermatitis, can disrupt the skin’s protective barrier, making it easier for bacteria to enter.
- Ingrown Hairs: Can lead to inflammation and secondary bacterial infections, increasing the risk of boil formation.
- Exposure to Harsh Chemicals: Frequent exposure to harsh chemicals or irritants can damage the skin and make it more vulnerable to infections.
Understanding these risk factors can help you take preventive measures to reduce your likelihood of developing boils.
 Close-up of a boil on the skin, showing redness and pus
Close-up of a boil on the skin, showing redness and pus
4. When Is It Time to See a Doctor About a Boil?
While small boils can often be treated at home, certain situations warrant medical attention. Here are key indicators for when to see a doctor about a boil:
- Large Size: Boils larger than 1/2 inch (1.25 cm) in diameter may require professional treatment.
- Location: Boils on the face, especially near the eyes or nose, can lead to serious complications and should be evaluated by a doctor.
- Severe Pain: Intense pain that doesn’t subside with over-the-counter pain relievers is a sign to seek medical help.
- Fever: A fever accompanying a boil indicates a more systemic infection that needs medical treatment.
- Spreading Infection: If the redness and inflammation spread beyond the immediate area of the boil, it could indicate cellulitis, a serious skin infection.
- No Improvement: If the boil doesn’t improve after a week of home treatment, it’s time to see a doctor.
- Recurrent Boils: Frequent boils may indicate an underlying health issue that requires medical evaluation.
- Underlying Health Conditions: People with diabetes, weakened immune systems, or other chronic conditions should seek medical attention for boils due to the higher risk of complications.
- Carbuncles: These large clusters of boils require professional medical intervention to prevent further spread of infection.
- Boil Does Not Drain: If the boil does not spontaneously drain within a few days, medical intervention may be needed to drain it safely.
4.1. Recognizing Signs of a More Serious Infection
Identifying signs that a boil has led to a more serious infection is critical. These signs include:
- Increased Pain and Tenderness: The area around the boil becomes increasingly painful and tender.
- Spreading Redness: The redness around the boil expands, indicating cellulitis.
- Swollen Lymph Nodes: Swollen lymph nodes in the groin, armpit, or neck can indicate the infection is spreading.
- Fever and Chills: These systemic symptoms suggest the infection has entered the bloodstream.
- Fatigue: Feeling unusually tired or weak can be a sign of a more serious infection.
- Pus or Drainage: An increase in pus or foul-smelling drainage from the boil.
- Red Streaks: Red streaks emanating from the boil could indicate blood poisoning and need immediate attention.
4.2. The Importance of Seeking Timely Medical Attention
Seeking medical attention when necessary can prevent complications and ensure proper treatment. Delaying treatment can lead to:
- Spread of Infection: Untreated boils can lead to the spread of infection to other parts of the body.
- Scarring: Improperly treated boils can result in significant scarring.
- Sepsis: In rare cases, a boil can lead to sepsis, a life-threatening blood infection.
- Cellulitis: The surrounding skin can become infected, leading to cellulitis, which requires antibiotic treatment.
- Osteomyelitis: In rare cases, the infection can spread to the bone, causing osteomyelitis.
- Endocarditis: The infection can also spread to the heart, causing endocarditis, a severe condition.
5. What to Expect During a Doctor’s Visit
When you see a doctor about a boil, you can expect a thorough examination and discussion of treatment options.
5.1. Diagnostic Procedures
The doctor will likely:
- Physical Examination: Examine the boil to assess its size, location, and severity.
- Medical History: Ask about your medical history, including any underlying conditions or medications you’re taking.
- Swab Culture: Take a sample of the pus to identify the bacteria causing the infection.
- Blood Tests: In severe cases, blood tests may be ordered to check for systemic infection.
5.2. Treatment Options Your Doctor May Recommend
Based on the diagnosis, the doctor may recommend one or more of the following treatments:
- Incision and Drainage (I&D): The doctor will make a small incision to drain the pus from the boil.
- Antibiotics: Oral or topical antibiotics may be prescribed to fight the bacterial infection.
- Wound Care: Instructions on how to keep the area clean and covered to promote healing.
- Pain Management: Recommendations for over-the-counter or prescription pain relievers.
- Follow-Up Appointments: Scheduled follow-up visits to monitor healing and ensure the infection is resolving.
- Referral to a Specialist: In complex cases, a referral to a dermatologist or infectious disease specialist may be necessary.
6. Home Care for Minor Boils: What You Can Do
For small, uncomplicated boils, home care can be effective.
6.1. Effective Home Remedies
- Warm Compresses: Applying warm compresses for 10-15 minutes several times a day can help draw the infection to the surface and promote drainage.
- Keep the Area Clean: Gently wash the boil and surrounding area with soap and water.
- Avoid Squeezing: Do not squeeze or pop the boil, as this can spread the infection.
- Over-the-Counter Pain Relief: Use over-the-counter pain relievers like ibuprofen or acetaminophen to manage pain.
- Topical Antibiotic Ointments: Applying a topical antibiotic ointment can help prevent secondary infections.
- Turmeric Paste: Turmeric has anti-inflammatory and antiseptic properties that may help reduce inflammation and promote healing.
- Tea Tree Oil: Diluted tea tree oil can be applied to the boil due to its antibacterial properties, but use with caution as it can irritate some people’s skin.
6.2. When Home Treatment Is Not Enough
If you notice any of the following, it’s time to seek professional medical help:
- The boil does not improve after a week of home treatment.
- Symptoms worsen despite home care efforts.
- Signs of spreading infection develop.
- Severe pain persists.
7. Preventing Boils: Tips and Best Practices
Prevention is key to avoiding the discomfort and potential complications of boils.
7.1. Hygiene Practices
- Regular Hand Washing: Wash your hands frequently with soap and water, especially after touching potentially contaminated surfaces.
- Shower Regularly: Maintain good personal hygiene by showering regularly, especially after sweating.
- Avoid Sharing Personal Items: Do not share towels, razors, or clothing with others.
- Keep Wounds Clean: Clean and cover any cuts or scrapes immediately to prevent infection.
- Use Clean Workout Gear: Wash workout clothes and equipment regularly.
- Avoid Tight Clothing: Wear loose-fitting clothing to reduce friction and allow the skin to breathe.
7.2. Lifestyle Adjustments
- Balanced Diet: A healthy diet can support a strong immune system and help prevent infections.
- Stay Hydrated: Drinking plenty of water keeps your skin healthy and resilient.
- Manage Underlying Conditions: Keep conditions like diabetes under control to reduce your risk of skin infections.
- Avoid Irritants: Minimize exposure to harsh chemicals or irritants that can damage the skin.
- Reduce Friction: Use powder to reduce friction in areas prone to boils, such as the groin or underarms.
- Stress Management: Practice stress-reducing activities, as chronic stress can weaken the immune system.
8. Boils and Underlying Health Conditions
Certain health conditions can increase your susceptibility to boils and complicate their treatment.
8.1. Diabetes
People with diabetes are more prone to boils due to:
- Impaired Immune Function: High blood sugar levels can weaken the immune system.
- Poor Circulation: Reduced blood flow can impair the body’s ability to fight infection.
- Nerve Damage: Neuropathy can make it harder to detect minor skin injuries, leading to infections.
Managing diabetes through proper diet, exercise, and medication is essential for preventing boils. Regular foot and skin checks are also crucial to catch and treat any issues early.
8.2. Weakened Immune Systems
Conditions or treatments that weaken the immune system, such as HIV/AIDS, chemotherapy, or immunosuppressant medications, can increase the risk of boils.
Strategies to support the immune system include:
- Healthy Diet: Eat a balanced diet rich in vitamins and minerals.
- Adequate Sleep: Get enough rest to support immune function.
- Stress Management: Practice stress-reducing activities.
- Vaccinations: Stay up-to-date on vaccinations to prevent infections.
8.3. Skin Conditions
Pre-existing skin conditions can disrupt the skin’s protective barrier, making it easier for bacteria to enter.
Common skin conditions include:
- Eczema: Causes dry, itchy skin that can crack and become infected.
- Psoriasis: Leads to thick, scaly patches that can be prone to infection.
- Dermatitis: Inflames the skin, making it more vulnerable to bacteria.
Managing these conditions with appropriate skincare routines and medications can help prevent boils.
9. Potential Complications of Untreated Boils
Leaving boils untreated can lead to several complications.
9.1. Cellulitis
Cellulitis is a bacterial infection of the deeper layers of the skin. It can cause:
- Redness and Swelling: The skin around the boil becomes red, swollen, and painful.
- Warmth: The affected area feels warm to the touch.
- Fever: A fever may accompany the skin changes.
Prompt antibiotic treatment is necessary to prevent the infection from spreading further.
9.2. Sepsis
Sepsis is a life-threatening condition that occurs when the body’s response to an infection gets out of control. Symptoms include:
- High Fever: A temperature above 101°F (38.3°C).
- Rapid Heart Rate: A heart rate over 90 beats per minute.
- Rapid Breathing: A respiratory rate over 20 breaths per minute.
- Confusion: Altered mental status or disorientation.
Sepsis requires immediate medical attention, including intravenous antibiotics and supportive care.
9.3. Scarring
Boils, especially those that are large or improperly treated, can leave scars. Proper wound care and avoiding squeezing the boil can help minimize scarring.
9.4. Other Infections
In rare cases, untreated boils can lead to more serious infections, such as:
- Osteomyelitis: Infection of the bone.
- Endocarditis: Infection of the inner lining of the heart.
10. Finding a Specialist: When to See a Podiatrist
While general practitioners can often treat boils, a podiatrist can provide specialized care in certain situations.
10.1. What Is a Podiatrist?
A podiatrist is a medical doctor specializing in treating conditions of the foot, ankle, and lower leg. They have extensive training in:
- Foot and Ankle Surgery: Performing surgical procedures to correct deformities or treat injuries.
- Wound Care: Managing and treating wounds, including those caused by infections.
- Orthotics: Prescribing and fitting custom orthotics to support and correct foot problems.
- Diabetic Foot Care: Providing specialized care to prevent and manage foot complications related to diabetes.
10.2. Situations Where a Podiatrist Is Needed
You should consider seeing a podiatrist for a boil if:
- The boil is on your foot or ankle.
- You have diabetes or another condition that affects your feet.
- The boil is severe or not responding to treatment.
- You need specialized wound care.
Podiatrists are equipped to provide comprehensive care for foot-related infections, ensuring proper healing and preventing complications.
 Close-up of a doctor examining a patient's foot
Close-up of a doctor examining a patient's foot
11. Optimizing Your Health with thebootdoctor.net
Navigating the complexities of foot health can be overwhelming, but thebootdoctor.net is here to help. Our website offers a wealth of information and resources to support your foot care journey.
11.1. Comprehensive Articles and Guides
Explore our extensive library of articles and guides covering a wide range of foot-related topics, including:
- Common Foot Conditions: Learn about conditions like plantar fasciitis, bunions, and hammertoes.
- Treatment Options: Discover the latest treatments and therapies for various foot problems.
- Foot Care Tips: Get practical advice on maintaining healthy feet.
- Shoe Guides: Find the perfect shoes for your specific needs and activities.
Our content is carefully crafted by experts to provide you with accurate, up-to-date information.
11.2. Expert Advice and Recommendations
Benefit from the knowledge and experience of our team of podiatrists and foot care specialists. We offer:
- Expert Articles: Insights and advice from leading podiatrists.
- Product Reviews: Honest reviews of foot care products and devices.
- Personalized Recommendations: Tailored advice to address your specific concerns.
11.3. Community Support and Resources
Connect with others who share your interest in foot health. Our website features:
- Forums and Discussion Boards: Share your experiences and ask questions.
- Success Stories: Read inspiring stories of people who have overcome foot problems.
- Resource Directory: Find links to reputable organizations and resources related to foot health.
12. Conclusion: Taking Control of Your Skin Health
Knowing when to see a doctor about a boil is crucial for preventing complications and ensuring proper care. While minor boils can often be managed at home, it’s important to recognize the signs of a more serious infection and seek medical attention when necessary. thebootdoctor.net is dedicated to providing you with the information and resources you need to make informed decisions about your foot and skin health.
12.1. Final Thoughts on Boil Management
- Early Detection: Recognizing the symptoms of a boil early can help prevent complications.
- Proper Hygiene: Maintaining good hygiene is essential for preventing boils.
- Timely Medical Care: Don’t hesitate to seek medical attention when necessary.
- Comprehensive Resources: Utilize the resources available at thebootdoctor.net to stay informed and proactive about your health.
12.2. Call to Action
Take the first step towards healthier feet and skin today. Visit thebootdoctor.net to explore our comprehensive resources, read expert articles, and connect with our community. If you have concerns about a boil or other foot-related issues, contact us for personalized advice and recommendations. Your journey to optimal foot health starts here!
Frequently Asked Questions (FAQs)
1. Can I treat a boil at home?
Yes, small boils can often be treated at home with warm compresses and proper hygiene. However, larger or more severe boils require medical attention.
2. When should I see a doctor about a boil?
See a doctor if the boil is large, located on your face, causes severe pain, is accompanied by a fever, shows signs of spreading infection, or doesn’t improve after a week of home treatment.
3. What causes boils?
Boils are primarily caused by bacterial infections, most commonly Staphylococcus aureus, which enter the body through breaks in the skin or hair follicles.
4. How can I prevent boils?
Prevent boils by practicing good hygiene, washing hands regularly, avoiding sharing personal items, and keeping wounds clean.
5. Are boils contagious?
Yes, boils are contagious. Avoid close contact with others and do not share personal items to prevent the spread of infection.
6. Can diabetes increase my risk of getting boils?
Yes, diabetes can increase your risk of getting boils due to impaired immune function and poor circulation.
7. What is incision and drainage (I&D)?
Incision and drainage is a procedure where a doctor makes a small cut in the boil to drain the pus.
8. What are the potential complications of untreated boils?
Potential complications include cellulitis, sepsis, scarring, and other infections.
9. Can a podiatrist help with boils?
Yes, a podiatrist can provide specialized care for boils, especially those on the foot or ankle.
10. Where can I find more information about foot health?
Visit thebootdoctor.net for comprehensive articles, expert advice, and community resources related to foot health.

