Are Doctors Notified When Prescriptions Are Filled? Yes, doctors can often track if you’ve filled your prescription through various means, including Electronic Health Records (EHRs) and pharmacy communication. At thebootdoctor.net, we aim to provide you with comprehensive insights into healthcare practices and how they impact your well-being, especially concerning foot health and related medical treatments. Understanding how your prescription information is shared can empower you to take better control of your health. To improve your foot health, explore preventative measures, potential treatments, and healthcare provider communication strategies.
1. What Is an Electronic Health Record (EHR) and How Does It Work?
Yes, Electronic Health Records (EHRs) allow doctors to see if a prescription has been filled. EHRs are digital versions of patients’ paper charts, offering a real-time, patient-centered record that makes information available instantly and securely to authorized users.
EHRs go beyond basic clinical data and typically include:
- Tools for healthcare providers to make informed decisions about patient care.
- Streamlined workflows through automation of processes.
- Comprehensive details including treatment plans, medications, immunizations, medical history, diagnoses, lab results, allergies, and radiology images.
According to HealthIT.gov, “One of the key features of an EHR is that health information can be created and managed by authorized providers in a digital format capable of being shared with other providers across more than one health care organization.” This interoperability ensures that all clinicians and health providers involved in a patient’s care can access and share information, including:
- Emergency facilities
- Laboratories
- Specialists
- Medical imagery providers
- Pharmacies
- Work and school medical clinics
EHRs enhance coordination and continuity of care, ensuring that healthcare providers have a complete view of a patient’s medical history and current treatments.
2. How Long Do Pharmacies Keep Prescription Records?
Yes, pharmacies keep prescription records for a certain amount of time. Here’s a breakdown of how long pharmacies typically retain different types of records, according to guidelines:
| Record Type | Description | Retention Period |
|---|---|---|
| Prescriptions | A hard copy record of a prescription. | 42 months, or 2 years past the completion of therapy. |
| Patient Record | Contains demographics, drug profile, and record of care provided. | 10 years past the last date of pharmacy service provided, or 2 years past the age of majority. |
| Record of Care | Includes records of drug therapy, problems, interventions, monitoring, prescriptions (filled and not filled), and summaries of consultations. | 10 years past the last date of pharmacy service provided, or 2 years past the age of majority. |
| Drug Error | Incidents and adverse drug effects, adverse outcomes. | 10 years after the error is discovered. |
| Health Info Disclosure | Records of diagnosis, treatment, and care, or records of information shared with other health organizations. | 10 years following the date of disclosure. |
| Narcotic Receipts | Records of narcotics received at a pharmacy or licensed outlet, such as a wholesaler. | 2 years from the date of the receipt. |
If a physician provides a patient with a handwritten prescription, the physician can contact the pharmacy to confirm whether the prescription was filled. With electronic prescriptions (e-prescriptions or e-Rx), the system often notifies the doctor whether the prescription has been picked up, not picked up, or partially filled.
3. What Other Ways Can Doctors Track Medication?
Yes, doctors have other ways to track your medication. Many states have established databases to monitor opioid and narcotic drug prescriptions. These databases track:
- Doctors’ prescription-writing habits.
- Pharmacy prescription-dispensing activities.
- Patients’ prescription filling.
When a patient sees their doctor and there’s a possibility of prescribing a pain-relieving drug, the doctor can access the database to ensure the patient isn’t “doctor shopping” to amass more drugs than legally or medically necessary, which could be dangerous. Discussions are ongoing to share this information across state lines, preventing patients from seeking prescriptions in multiple states.
While some patients worry about privacy, these databases help doctors prescribe drugs more confidently to appropriate patients, reducing the risk of legal issues. Emergency room personnel can also access these databases to avoid prescribing conflicting medications or dismissing patients who have sought emergency care.
Additionally, these systems help identify patients who may be overusing pain-relieving drugs, encouraging them to wean off these medications when appropriate. Doctors gain a comprehensive view of a patient’s pain drug history, including prescriptions from other doctors.
4. Why Don’t People Fill Their Prescriptions?
There are several reasons why patients might not fill their prescriptions. According to the NCBI, approximately 50% of patients do not take their medications as prescribed. Common reasons include:
- Cost: Affordability issues may prevent patients from filling prescriptions or lead them to reduce dosages to extend their supply.
- Fear: Concerns about potential side effects, based on personal experiences or stories from others, can deter patients from filling prescriptions.
- Misunderstanding: Patients may not understand the need for the medication or believe it’s unnecessary for improving their health, especially with chronic conditions where immediate improvements aren’t apparent.
- Too many medications: The more medications prescribed and the higher the dosing frequency, the more likely a patient is to be non-adherent.
- Lack of symptoms: If symptoms disappear, patients may believe they no longer need the medication.
- Denial: Patients may believe the illness will resolve on its own without medication.
- Worry: Concerns about dependency can make patients reluctant to start a medication.
- Depression: Depression can diminish the importance placed on health issues, reducing the likelihood of filling prescriptions.
- Mistrust: Patients may doubt their doctor’s diagnosis or motives for prescribing certain medications, influenced by personal beliefs, news reports, or concerns about pharmaceutical company influence.
Dr. Michael A. Fischer from Brigham and Women’s Hospital advises, “If you are not sure why you are being prescribed a medication, ask your doctor directly. One of our jobs as physicians is to educate and advise our patients.” Always discuss any uncertainties about your prescriptions with your doctor.
5. What Are the Consequences of Not Filling Prescriptions?
Not filling prescriptions, also known as medical non-adherence, can have significant health and economic consequences. The National Council on Patient Information and Education found that as many as half of all patients do not follow their doctors’ medication advice. Patients with long-term conditions like high blood pressure and diabetes who do not adhere to their prescriptions are more likely to become sicker, have higher mortality rates, and suffer more complications.
The economic impact of medication non-adherence is staggering, costing over $170 billion each year in the United States, with some reports estimating as high as $300 billion.
Recent research highlights that non-adherence can begin even before a prescription is filled. A Harvard Medical School study found that over 20% of first-time prescriptions are never filled. Prescriptions for chronic diseases like high cholesterol, high blood pressure, and diabetes are less likely to be filled compared to those for pediatric patients or antibiotics.
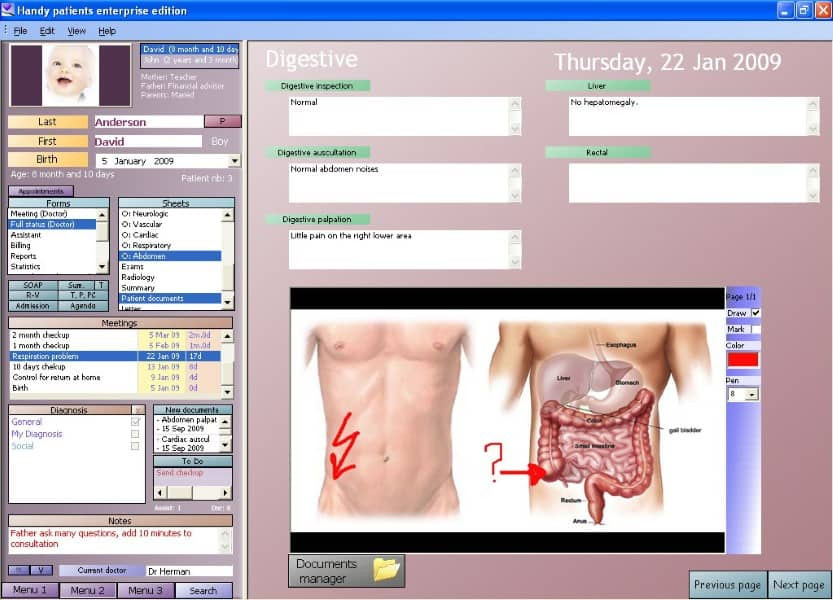
 Doctor checking prescription
Doctor checking prescription
6. How Can Electronic Prescriptions (E-Prescriptions) Help Doctors?
Yes, Electronic prescriptions (e-prescriptions or e-Rx) offer several benefits to doctors. They can enhance the prescription process and improve patient care. Here’s how:
- Improved Accuracy: E-prescriptions reduce the risk of errors associated with handwritten prescriptions, such as illegible handwriting or misinterpretation of drug names and dosages.
- Enhanced Safety: E-prescribing systems often include built-in checks for drug interactions, allergies, and appropriate dosages, alerting the physician to potential issues before the prescription is sent.
- Streamlined Workflow: E-prescriptions can be sent directly to the pharmacy, saving time for both the patient and the doctor’s office. This eliminates the need for patients to drop off or mail in prescriptions.
- Better Tracking: Doctors can receive notifications about whether a patient has picked up their prescription, allowing for timely follow-up if a patient does not fill their medication.
- Reduced Fraud and Abuse: E-prescriptions help prevent prescription fraud and abuse by creating an electronic audit trail and making it more difficult for unauthorized individuals to alter or forge prescriptions.
- Integration with EHRs: E-prescriptions are integrated with Electronic Health Records (EHRs), providing a comprehensive view of a patient’s medication history and overall health status.
According to a study published in the Journal of the American Medical Informatics Association, e-prescribing is associated with a significant reduction in medication errors and improved adherence to prescribing guidelines.
7. What Role Do State Prescription Drug Monitoring Programs (PDMPs) Play?
Yes, State Prescription Drug Monitoring Programs (PDMPs) play a crucial role in tracking and monitoring the prescribing and dispensing of controlled substances. These programs help to:
- Prevent Doctor Shopping: PDMPs allow doctors to check a patient’s prescription history to identify individuals who may be obtaining controlled substances from multiple providers, a practice known as “doctor shopping.”
- Reduce Drug Diversion: By tracking prescriptions, PDMPs help to identify and prevent the diversion of controlled substances for illegal use or sale.
- Improve Patient Safety: PDMPs provide doctors with valuable information about a patient’s medication history, allowing them to make more informed decisions about prescribing controlled substances.
- Support Law Enforcement: PDMPs provide law enforcement agencies with data to investigate and prosecute cases of prescription drug fraud and abuse.
The Centers for Disease Control and Prevention (CDC) recognizes PDMPs as an effective tool in addressing the opioid crisis. According to the CDC, “PDMPs are electronic databases that track controlled substance prescriptions dispensed in a state. They can provide valuable information to help reduce prescription drug misuse and diversion.”
8. How Does Patient Privacy Factor into Prescription Tracking?
Yes, patient privacy is a critical consideration in prescription tracking. Healthcare providers and pharmacies must adhere to strict privacy regulations, such as the Health Insurance Portability and Accountability Act (HIPAA), to protect patient information. Key aspects of patient privacy in prescription tracking include:
- HIPAA Compliance: Healthcare providers must comply with HIPAA regulations, which protect the privacy and security of patient health information.
- Data Security: Pharmacies and healthcare providers must implement security measures to protect prescription data from unauthorized access, use, or disclosure.
- Limited Access: Access to prescription information is limited to authorized healthcare professionals who are involved in the patient’s care.
- Patient Consent: In some cases, healthcare providers may need to obtain patient consent before accessing or sharing prescription information.
The U.S. Department of Health and Human Services (HHS) provides detailed information on HIPAA regulations and patient privacy rights. According to HHS, “The HIPAA Privacy Rule establishes a national standard for the protection of individually identifiable health information.”
9. What Are Some Alternatives If I Can’t Afford My Medications?
Yes, If you’re struggling to afford your medications, several options can help. Some alternatives include:
- Generic Medications: Generic drugs are typically less expensive than brand-name medications and contain the same active ingredients.
- Prescription Assistance Programs: Many pharmaceutical companies offer patient assistance programs that provide free or discounted medications to eligible individuals.
- Discount Cards and Coupons: Numerous websites and organizations offer prescription discount cards and coupons that can lower the cost of medications.
- State and Local Programs: Some states and local communities offer programs that provide assistance with prescription drug costs.
- Discuss with Your Doctor: Talk to your doctor about alternative medications or treatment options that may be more affordable.
Organizations like RxAssist and NeedyMeds provide comprehensive resources for finding affordable medications and assistance programs.
10. How Can thebootdoctor.net Help Me Understand and Manage My Foot Health?
Thebootdoctor.net is dedicated to providing reliable and accessible information about foot health. Our website offers:
- Detailed Articles: Comprehensive articles on various foot conditions, treatments, and preventative measures.
- Expert Advice: Insights and recommendations from foot care professionals to help you make informed decisions.
- Product Reviews: Honest reviews of footwear and foot care products to help you choose the best options for your needs.
- Community Forum: A platform to connect with others, share experiences, and ask questions about foot health.
Whether you’re dealing with plantar fasciitis, bunions, diabetic foot issues, or simply looking for the best shoes for your feet, thebootdoctor.net is your go-to resource for all things foot health.
 electronic health record
electronic health record
In conclusion, doctors have various methods to track medication adherence, from EHRs to state monitoring programs, ensuring informed and safe patient care. Always discuss any concerns about your prescriptions or foot health with healthcare professionals, and explore resources like thebootdoctor.net for reliable information and support.
Are you experiencing foot pain or discomfort? Visit thebootdoctor.net today for expert advice, product recommendations, and resources to help you achieve optimal foot health. Our team of professionals is dedicated to providing you with the highest quality information and care. Contact us at Address: 6565 Fannin St, Houston, TX 77030, United States. Phone: +1 (713) 791-1414 or visit our website thebootdoctor.net to schedule a consultation and take the first step toward healthier feet.
FAQ: Frequently Asked Questions About Prescription Tracking
1. Can my doctor see all the medications I’ve been prescribed, even by other doctors?
Yes, through Electronic Health Records (EHRs) and state Prescription Drug Monitoring Programs (PDMPs), your doctor can often see a comprehensive list of medications prescribed by various healthcare providers.
2. Is it legal for doctors to track my prescriptions?
Yes, it is legal for doctors to track your prescriptions, provided they adhere to HIPAA regulations and use this information to ensure safe and effective patient care.
3. How do I find out if my doctor is tracking my prescriptions?
Ask your doctor directly about their practices for monitoring prescriptions. They should be transparent about how they use EHRs and PDMPs to manage your care.
4. What if I don’t want my doctor to see my prescription history?
You can discuss your concerns with your doctor, but keep in mind that this information is crucial for your safety and well-being. Refusing access might impact the quality of care you receive.
5. Are over-the-counter medications tracked in the same way as prescriptions?
No, over-the-counter medications are generally not tracked in the same way as prescriptions, as they do not require a prescription from a doctor.
6. Can insurance companies see if I’ve filled my prescriptions?
Yes, insurance companies can typically see if you’ve filled your prescriptions as part of processing claims and managing healthcare benefits.
7. What are the benefits of doctors tracking prescriptions for patients with foot conditions?
Tracking prescriptions helps manage pain, prevent drug interactions, and ensure adherence to treatment plans, which is especially important for conditions like diabetic neuropathy or post-surgical care.
8. How does prescription tracking affect patients with chronic pain?
It helps ensure they are receiving appropriate pain management while minimizing the risk of drug abuse or dependence, and avoiding potentially dangerous drug interactions.
9. What should I do if I can’t afford a medication prescribed for a foot condition?
Discuss alternatives with your doctor, such as generic options, patient assistance programs, or using discount cards. Websites like RxAssist and NeedyMeds can also provide resources.
10. Where can I find reliable information about foot health and medication management?
thebootdoctor.net offers expert advice, detailed articles, and product reviews to help you understand and manage your foot health. Consult healthcare professionals for personalized guidance.
